1) Welcome to a new #accredited #tweetorial entitled "#HeartFailure & #KidneyDisease: The Next Epidemics." Our expert faculty is Ahmed Mohsen @drahmedmohsen85, cardiologist at @CairoUniv 🇪🇬

2) Dr. Mohsen is also Ambassador for Africa in Tele-Cardiology Working group (ISfTeH) and is author of the book, Tips and Tricks in Cardiology. This program is accredited for 0.75 h credit for #physicians #physicianassociates #nursepractitioners #nurses #pharmacists.
3) This program is intended for #healthcare providers & is supported by an educational grant from AstraZeneca Pharmaceuticals. Faculty disclosures listed at https://cardiometabolic-ce.com/disclosures/. Join so many of your #CaReMe colleagues & FOLLOW US for outstanding programs from experts🌎🌍🌏
4) #Cardiovascular disease in patients with #CKD is more frequent, more severe, & has different manifestations compared w/ the non-CKD population➡️high economic & societal burden.
5) Although the risk of conventional atherosclerotic events⬆️when kidney function is⬇️, most of the excess #CV risk associated w/ #CKD is due to non-atherosclerotic pathologies, such as left ventricular hypertrophy (#LVH) with diastolic & systolic dysfunction, dysrhythmia, …
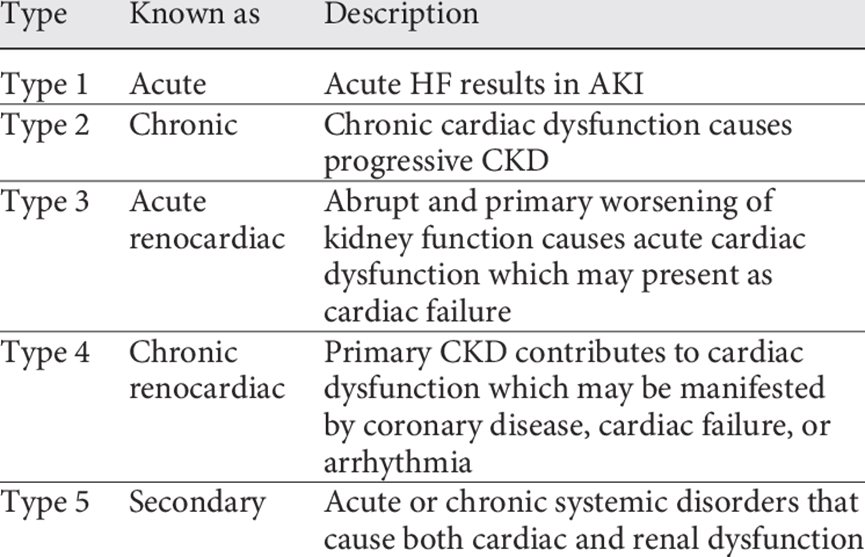
6) … sudden cardiac death, cardiac valve disease, arterial calcification, and hemorrhagic stroke. Either ischemic or non-ischemic cardiac diseases present in CKD patients are characterized by evolving to chronic congestive heart failure (HF) (i.e., cardiorenal syndrome type 4).
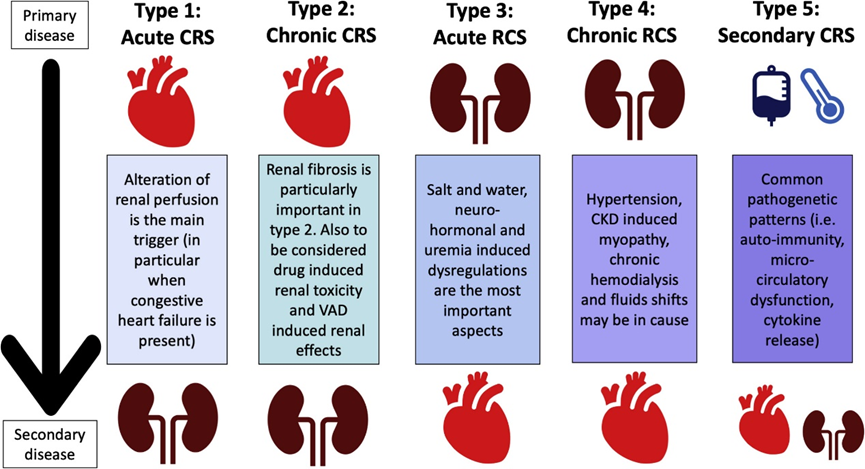
7) Of note, the⬆️death rates associated with all stages of CKD might reflect accelerated rates of both atherosclerosis & HF . . . but pts w/primary 🫀 disease & #HF can experience secondary ⬇️kidney function. Both can coexist based on shared risk factors or systemic disorders.
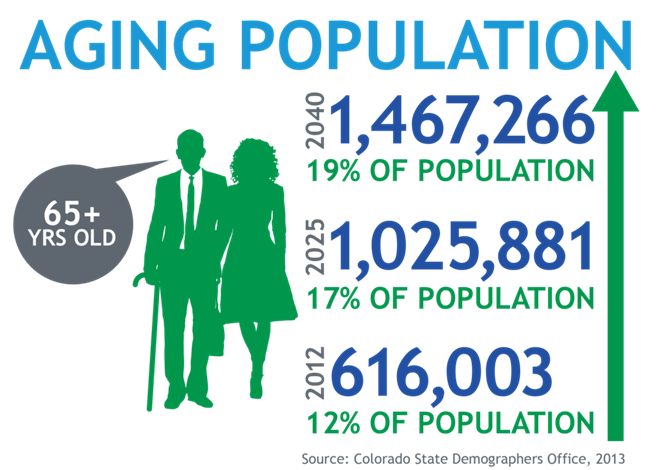
8) No doubt, combo of CKD & HF is a growing health, economical & societal problem as the aging population ➡️⬆️numbers of affected ppl. Pts w/both #CKD & and #HF experience unacceptably high rates of symptom load, hospitalization, & mortality.
9) @drahmedmohsen85 shares these references of interest from this introduction:
🔓https://pubmed.ncbi.nlm.nih.gov/31901373/
🔓https://pubmed.ncbi.nlm.nih.gov/21750584/
🔓https://pubmed.ncbi.nlm.nih.gov/31053387/
🔓
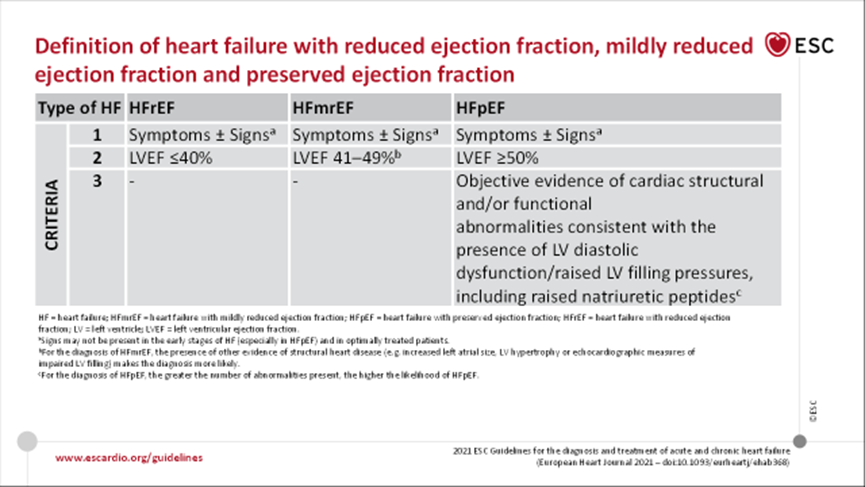
10) So now let's establish some definitions so that we are all speaking in the same terms. First, #heartfailure, from 🔓https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Acute-and-Chronic-Heart-Failure:
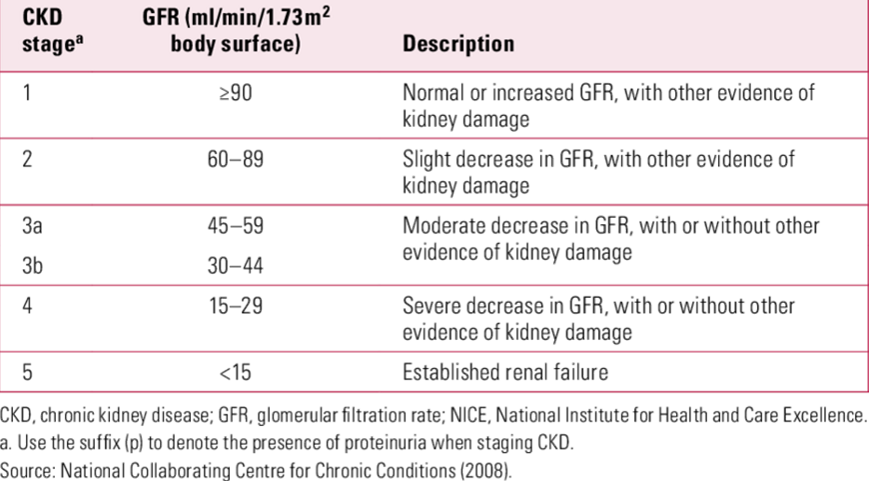
11) Per @goKDIGO at 🔓https://kdigo.org/guidelines/ckd-evaluation-and-management/, #CKD is defined on the basis of persistently reduced estimated glomerular filtration rate of <60 ml/min per 1.73 m2 or at least 1 marker of kidney damage for >3 months.
12) The latter markers include albuminuria, urine sediment abnormalities, histological, or structural abnormalities.
And #CKD is graded in stages, allowing us to know that we are comparing 🍎to 🍎:
13) So what do you know? What is the most accurate expression of the approximate prevalence of moderate to severe kidney impairment (defined as a #GFR < 60 mL/min per 1.73 m2) in patients with #heartfailure?
14) Different databases tell us different numbers, but the best answer is ~ 30-60 percent. In a systematic review of 16 studies of > 80,000 hosp and non-hosp pts with HF, moderate to severe kidney impairment (eGFR < 53 mL/min, serum creat > 1.5 mg/dL+, or …

15) …serum cystatin C > 1.56 mg/dL+ ) was present in 29% of pts. In the Acute Decompensated Heart Failure National Registry (ADHERE) database of > 100,000 pts w/HF req'ing hospitalization, ~30% had #CKD (defined as serum creat > 2.0 mg/dL).
16) In ADHERE, mean eGFR was 55 mL/min per m2, & only 9% had normal eGFR (defined as at least 90 mL/min per 1.73 m2). In addition to these baseline observations, pts under tx for acute or chronic #HF frequently develop⬆️serum creat, fulfilling criteria for type 1 or type 2 #CRS.
17) In different series, ~ 20-30% of patients developed ⬆️serum creat > 0.3 mg/dL. In one report, 24% had⬆️of 0.5 mg/dL+. Risk factors for worsening kidney function during admission for HF include which of the following?
Mark your answer BEFORE you scroll ⤵️!!
18) It's d, prior history of HF or diabetes & uncontrolled #hypertension, and also an admission serum creatinine of 1.5 mg/dL or higher. The⬆️in serum creat usually occurs in the first 3-5 days of hospitalization. It is known that 1/2 – 2/3 of pts w/HF present with eGFR < 60, …
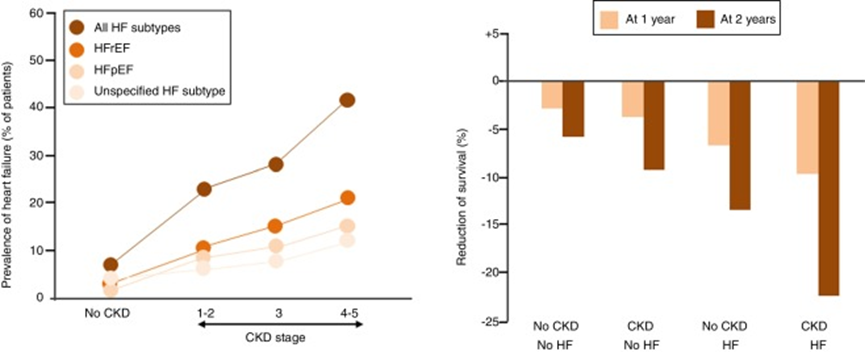
19) … w/ a greater prevalence in those with more severe symptoms & a stepwise⬆️in mortality risk with ⬇️ eGFR. The epidemiological figures of HF in patients initially identified as having CKD are not so well known. 🤔
🔓https://pubmed.ncbi.nlm.nih.gov/22441773/
20) Per the US Renal Data System (🔓https://www.usrds.org/media/1621/v2_c09_cvd_16.pdf), in 2016, the prevalence of #HF in #CKD pts aged 65 and older was ~X%, compared to Y% among pts without CKD.
What are X and Y? MARK YOUR ANSWER before you scroll⤵️!
21) It's b, an awfully big delta! Going all the way to #ESKD, about 44% of those patients have #HF
— 10% with #HFpEF
— 13% with #HFrEF
— 21% with unspecified
22) So we have been drinking from the firehose here . . . let's take a break. PLEASE RETURN TOMORROW for more education on the looming dual epidemics of #CKD and #HF! Nods to @ValleAlfonso @GoggleDocs @mvaduganathan @SantosGallegoMD @gcfmd @BiykemB @kevin_damman @P_Rossing
23) WELCOME BACK! We're talking about the unfortunately parallel⬆️s in incidence #HF & #CKD, while you earn🆓CE/#CME taught by @drahmedmohsen85 🇪🇬. 👏to @AgarwalRajivMD @ErinMichos @ShelleyZieroth @EzequielZaidel @robmentz @edgarvlermamd @nephondemand @VietHeartPA
24) Whereas the worldwide incidence of de novo #HF in the general population does not exceed 1%, the incidence in known #CKD is ~ 17% – 21%. Bad things go together!
🔓https://pubmed.ncbi.nlm.nih.gov/28785469/
🔓
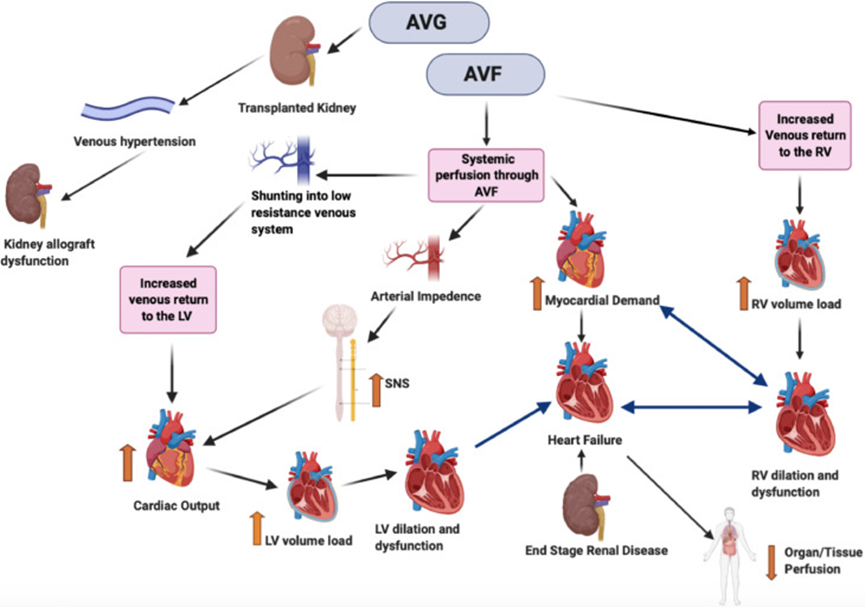
25) It gets even worse for pts w/ #ESKD. Evidence ➡️ in pts undergoing #hemodialysis & in pts S/P #kidneytransplant, the vascular access may be a risk factor for HF as high AV fistula flow is assoc'd w/LVH, LV dilatation, &⬇️#LVEF, + #PAH & #RV dysfunction.
26) In addition, through its effect as a left-to-right extracardiac shunt, the arteriovenous fistula can increase cardiac workload substantially, & in some pts ➡️high-output state & resultant HF over time.
🔓https://pubmed.ncbi.nlm.nih.gov/26299166/
https://pubmed.ncbi.nlm.nih.gov/20854331/
27) What about #prognosis? The presence of # HF ⬇️survival among patients both w/ & w/o #CKD, but more so with CKD (p-value for interaction <0.0001). See 🔓
28) Over 2y, pts w/ both CKD+HF had adjusted survival probability of 77.8%, vs 90.2% for those with CKD alone, & 93.7% for those without or CKD. 🔓https://www.usrds.org/media/1621/v2_c09_cvd_16.pdf. For which was #CKD more strongly associated with mortality & more prognostic discrimination?
29) It's HFrEF . . . and the association of CKD with mortality in HFrEF is independent of age, functional class, duration of HF, hemoglobin, or diabetes mellitus. See 🔓
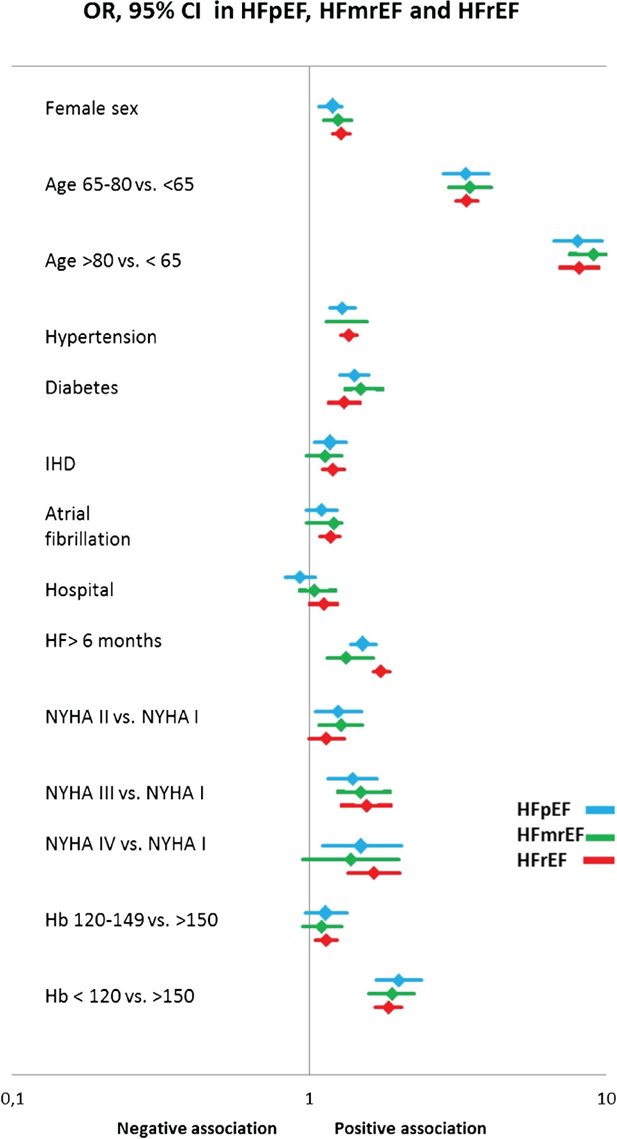
30) So what about diagnosing structural 🫀disease (such as #LVH) in pts w/ #CKD? Structural heart disease is highly prevalent in patients with CKD, the prevalence increasing progressively with the loss of renal function and thus is present in > 80% of patients with ESRD.

31) Hence, the ADQI XI Workgroup proposed a new definition of structural cardiac disease in #HF for pts w/ #CKD, namely for patients with #ESRD, according to the presence of at least 1⃣of 8⃣ #echocardiographic alterations (🔓https://pubmed.ncbi.nlm.nih.gov/24530671/).
32) So that's echo. What about lab values? How do we interpret Natriuretic Peptide (NP) levels in pts w/ #CKD?
CKD is one among the numerous causes of elevated NPs that may weaken their diagnostic utility in HF. See 🔓https://pubmed.ncbi.nlm.nih.gov/18760965/.
33) Current data➡️cause of elevated NP concentrations in advanced CKD is multifactorial, representing in part a true counter-regulatory response from the heart to the kidney–not only ⬇️passive renal clearance, as only 25% clearance of NPs is related to renal filtration.
34) Indeed, 2 recent studies➡️pts w/advanced #CKD + #HF w/⬆️#BNP have very low #neprilysin activity & postulated that BNP is a potent endogenous neprilysin inhibitor. See 🔓https://pubmed.ncbi.nlm.nih.gov/26251090/ & 🔓https://pubmed.ncbi.nlm.nih.gov/29635392/.
35) To maintain optimal diagnostic performance, the cut-off concentrations for detecting HF may need to be ⬆️when eGFR is <60. With strong correlation between renal dysfunction & age, no additional adjustment seems necessary for NT-proBNP once using age-adjusted rule-in cut-offs.
36) For #BNP, effect of renal dysfunction overall is smaller, & ⬆️the rule-out cut-off to 200 pg/mL rather than 100 pg/mL seems sufficient. Due to incomplete data, NP testing for #HF should be discouraged in pts on dialysis.
🔓https://pubmed.ncbi.nlm.nih.gov/19264247/
🔓
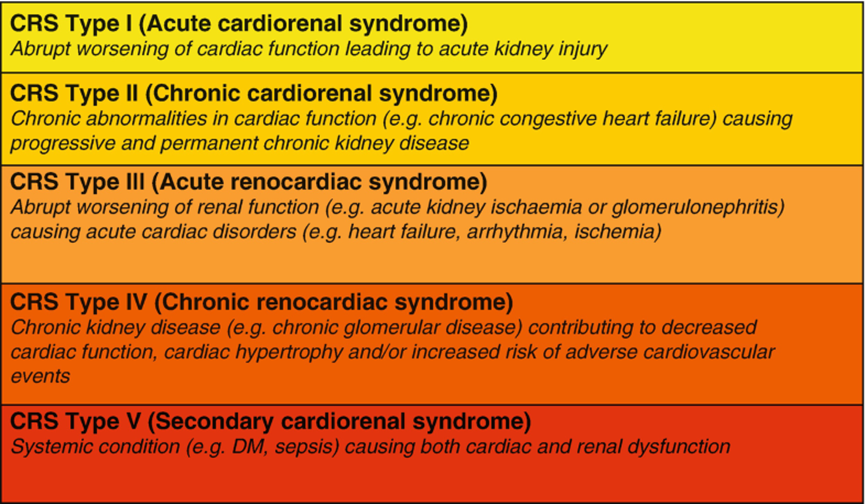
37) So we're here on @cardiomet_CE, which owes its existence to organ system interplay such as that seen in #cardiorenal syndrome.
🔓
38) So let's wind down this #tweetorial–and get to your CE/#CME credit grab, with a review of best management of #heartfailure in patients with #CKD.
🔓https://pubmed.ncbi.nlm.nih.gov/30123941/;
https://link.springer.com/article/10.1007/s00059-021-05024-3;
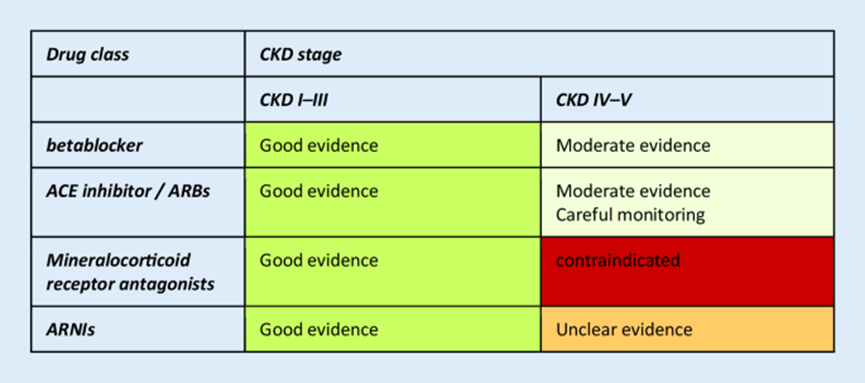
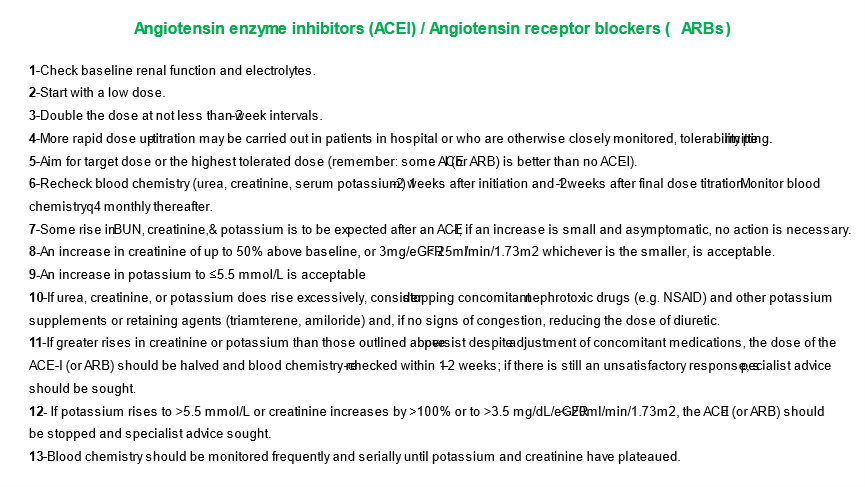
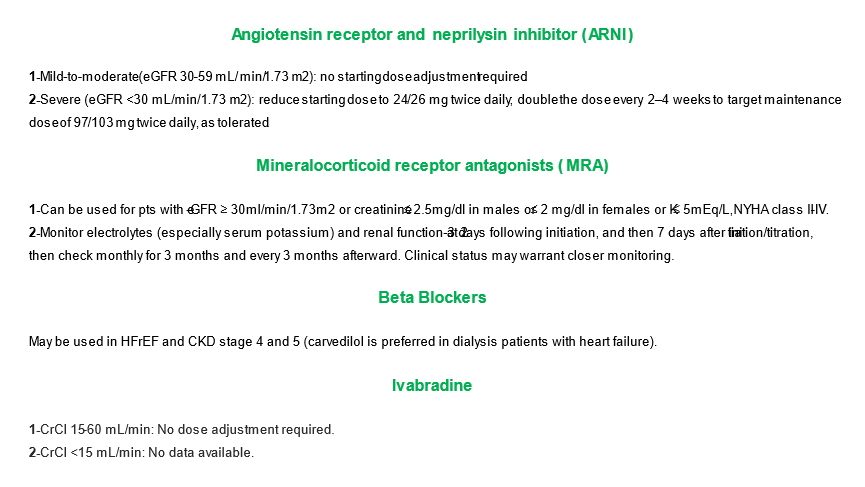
40) Re Angiotensin receptor and neprilysin inhibitor (#ARNI), mineralocorticoid receptor antagonists (BONUS: for more CE/CME, go to https://ckd-ce.com/category/mra/), beta blockers, & #ivabradine:
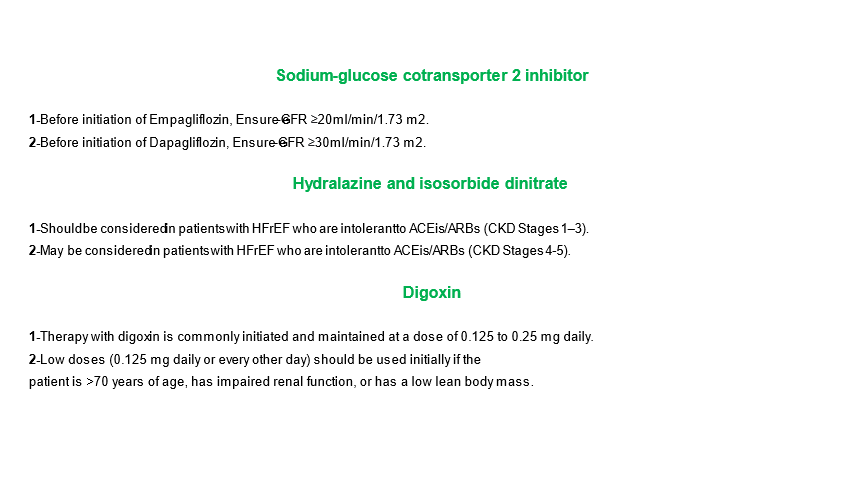
41) Re #SGLT2i, #hydralazine & #isosrbide, & #digoxin:
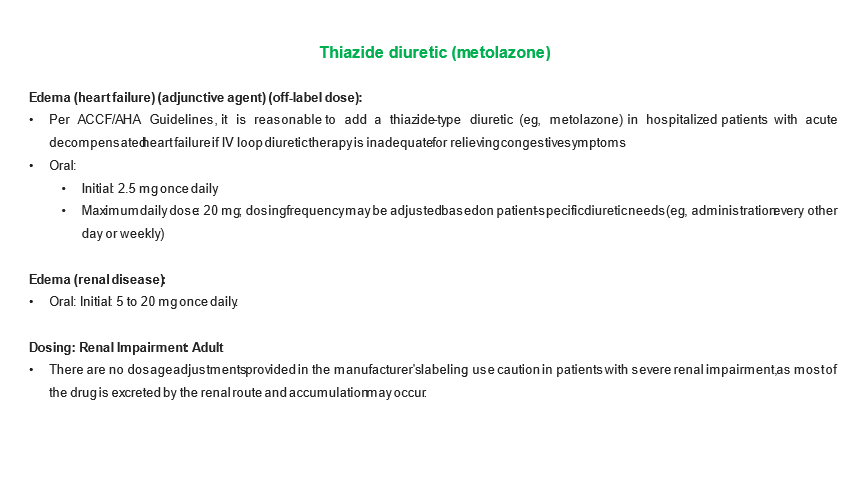
42) Finally, re diuretics in pts with #HF and #CKD:
43) And with that, you MADE IT! You're READY for the coming epidemics of #HF & #CKD! Go to https://cardiometabolic-ce.com/cardiorenal16/ & claim your credit: #physicians #physicianassoicates #pharmacists #nurses #nursepratitioners. I am @drahmedmohsen85. FOLLOW US for more expert-led CE/#CME programs!
Originally tweeted by cardio-met (@cardiomet_CE) on March 8, 2022.
