Here's something we only do rarely–joint posting of an #accredited #tweetorial on @cardiomet_CE and @ckd_ce at the same time. What's the 🗝️ this time? Anderson-#Fabry disease, which affects both the #cardiovascular and #renal organ systems. Figure from 🔓
1) Welcome to a #tweetorial on the diagnosis of & emerging treatment options for #Fabry disease. This program is accredited for 0.75 CE/#CME credits for #physicians #nurses #PAs #pharmacists by @academiccme! I am Ahmad Masri @MasriAhmadMD from @OHSUCardio.

2) This program is intended for healthcare professionals and is supported by an educational grant from Chiesi USA. Faculty disclosures are listed at http://cardiometabolic-ce.com/disclosures/. See archived programs, all by expert authors, still available for credit at http://cardiometabolic-ce.com.
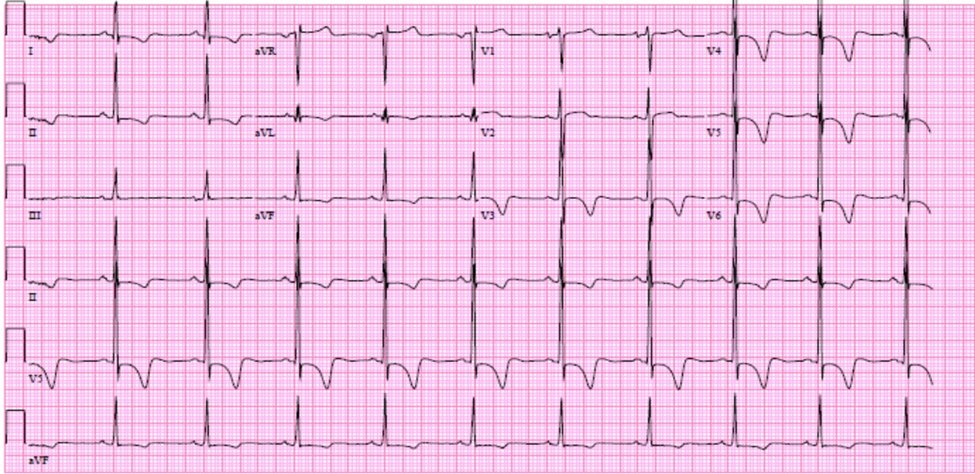
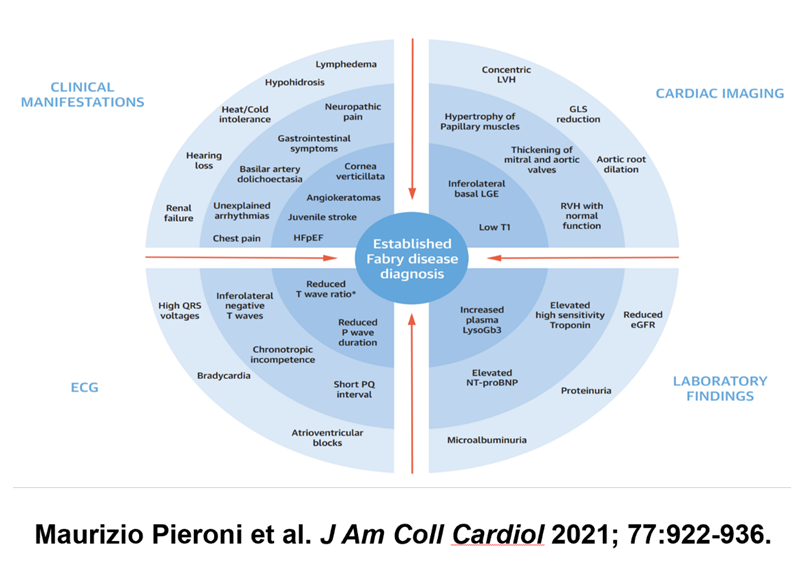
3) Let's start with a case: Caucasian 58♀️with exertional dyspnea x 12mo. No past medical history. BP in office 152/91. EKG shown. Echo showed moderate concentric #LVH with grade I diastolic dysfunction. Diagnosed with #hypertension & prescribed amlodipine.
4) Her daily blood pressure was controlled with amlodipine, averaging 125/75. She still complained of exertional dyspnea. Cardiac MR #whyCMR was obtained showing #LVH and inferolateral mid-myocardial enhancement upon late gadolinium enhancement (#LGE).
5) What other sequences should have been obtained as part of this #WhyCMR? Mark your answer before you scroll down!
A) Phase contrast (flow) imaging of the mitral valve
B) T1 and T2 mapping
C) Myocardial tagging sequence
D) Early gadolinium enhancement imaging
6) The answer is B. Enhancement is in a non-coronary (MI) distribution. The differential diagnosis includes (but not limited to) #Fabry disease, #sarcoidosis, #myocarditis.
🔓
7) T1 (tissue composition) and T2 (edema/water imaging) mapping, alongside LGE, allow for tissue characterization of the myocardium. T1 value is low in iron and fat/lipid deposition, while T2 is high in inflammation/edema.
8) T1 mapping showed a T1 relaxation time of 910 ms (normal range, magnet specific, 950-1050 ms) with a normal T2* (no iron) and elevated T2 relaxation time (edema).
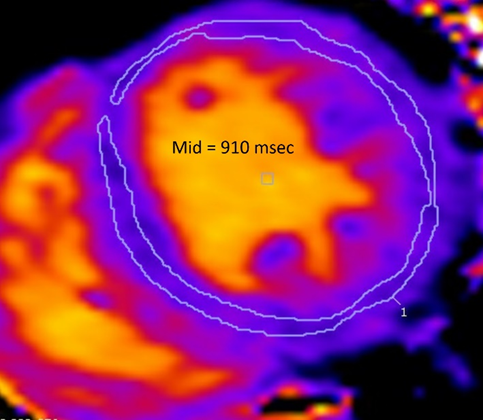
9) The constellation of #WhyCMR findings are concerning for #Fabry (FD or Anderson-Fabry) disease. Genetic testing showed a pathogenic mutation in the GLA gene. Baseline testing showed alpha-galactosidase<LLN, elevated plasma lyso- and urine GB3.
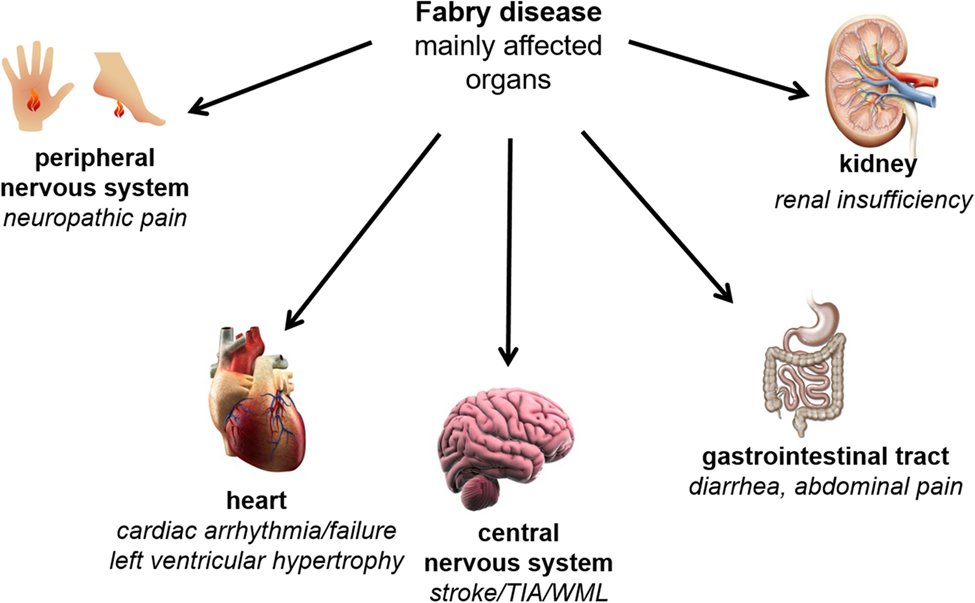
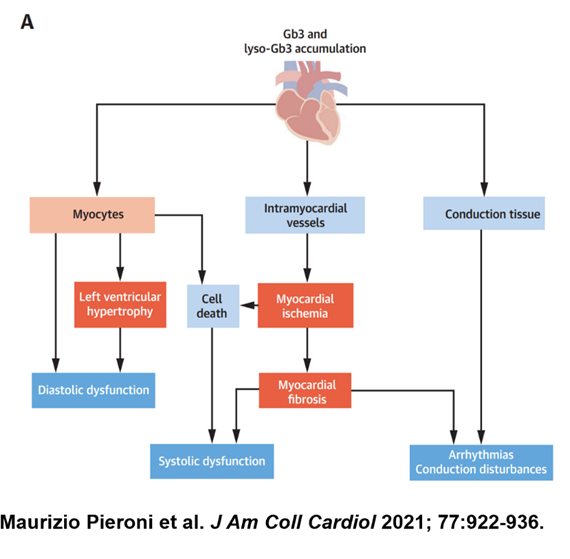
10) FD is the most prevalent lysosomal disease (X-linked). Pathogenic variants in the GLA gene lead to decrease alpha-galactosidase A (AGalA) activity. FD most commonly affects heart, kidneys, vasculature, and PNS.
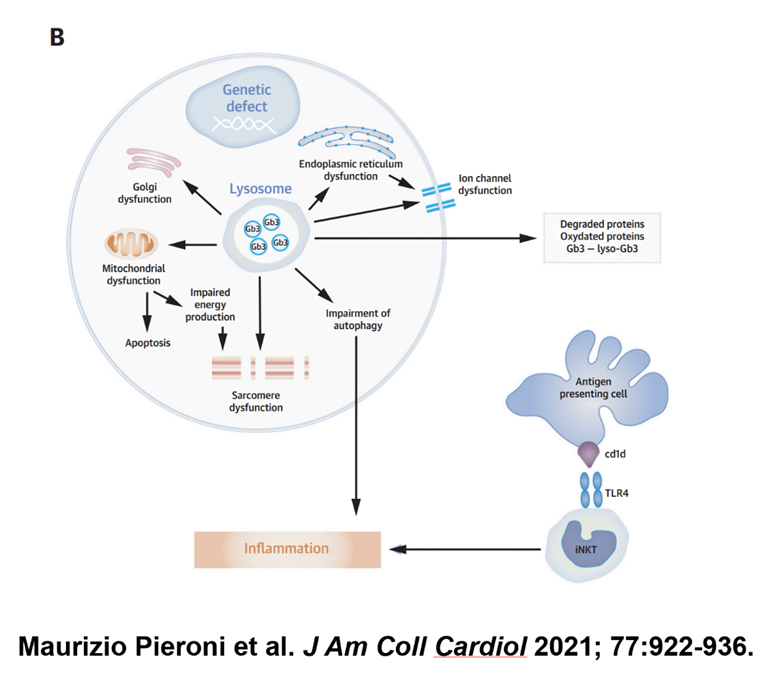
11) Decreased #AGalA activity leads to accumulation of globotriaosylsphingosine (lysoGB3) which in turn has adverse effects. Many other secondary pathways have been implicated.
12) FD is more common that originally described. Classically, it is thought to affect 1/40,000 males but newborn screening studies estimate 1/3000-8000 prevalence. As the above case illustrates, FD is largely underdiagnosed.
13) In one registry, median onset of symptoms to diagnosis was 11 years in both sexes.
🔓
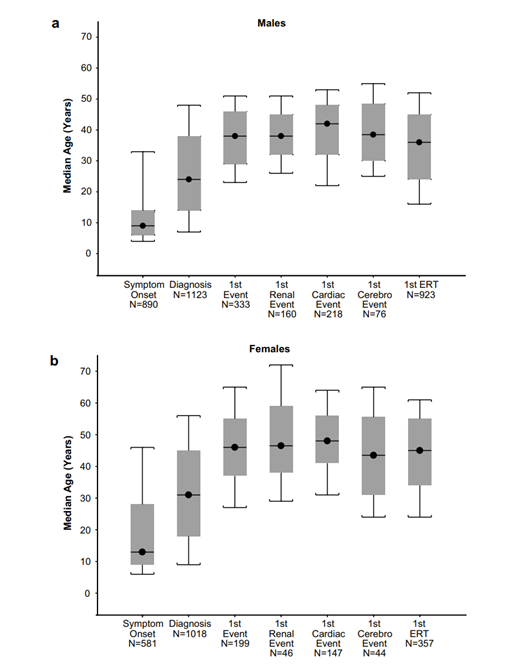
14) FD can be early onset (classic ♂️) or late onset (usually ♀️ w/heterogenous manifestation from nonrandom inactivation of X chromosome w/the mutation expressed in affected organs. Our patient had 🚩: acroparesthesia (neuropathic pain), #proteinuria (0.5g/24h) & #ECG short PR.
15) Which of the following #FD manifestations was first described in 1898?
A) Acroparesthesia
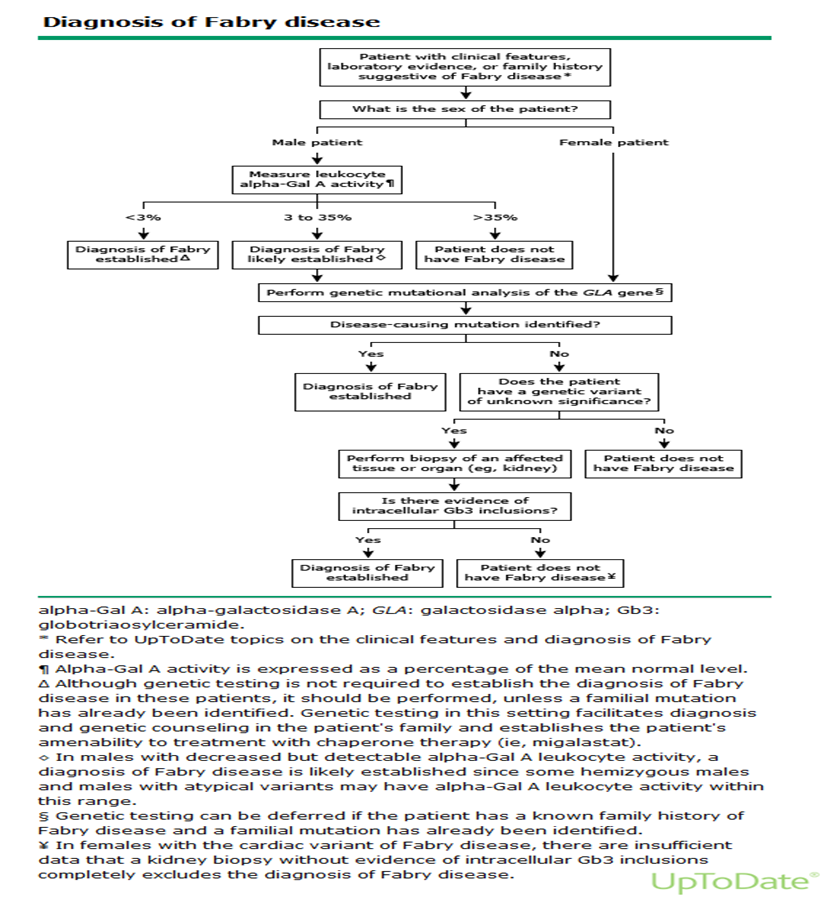
B) Angiokeratoma
C) Hypohydrosis
D) Cornea Verticillata
16) The answer is B. Anderson W: A case of “angeiokeratoma”. Br J Dermatol 10: 113–117, 1898. Cornea Verticillata is whorl-like pattern of golden brown or gray opacities in the cornea
17) In the heart, GB3 accumulation affects the myocytes, blood vessels and conduction system #CardioTwitter #FOAMed
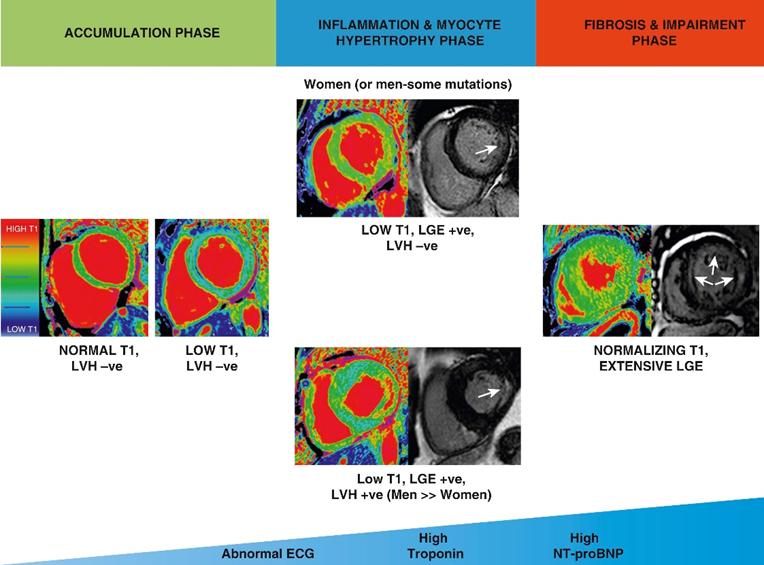
18) #WhyCMR has helped delineate the different stages of FD and predict response to therapy in patients based on their stage. 🔓
19) It is essential to keep in mind that #FD affects the vasculature. Patients can have #LVH/#CKD and significant #hypertension. A thorough clinical assessment and heightened index of suspicion is required to diagnose FD in such patients.
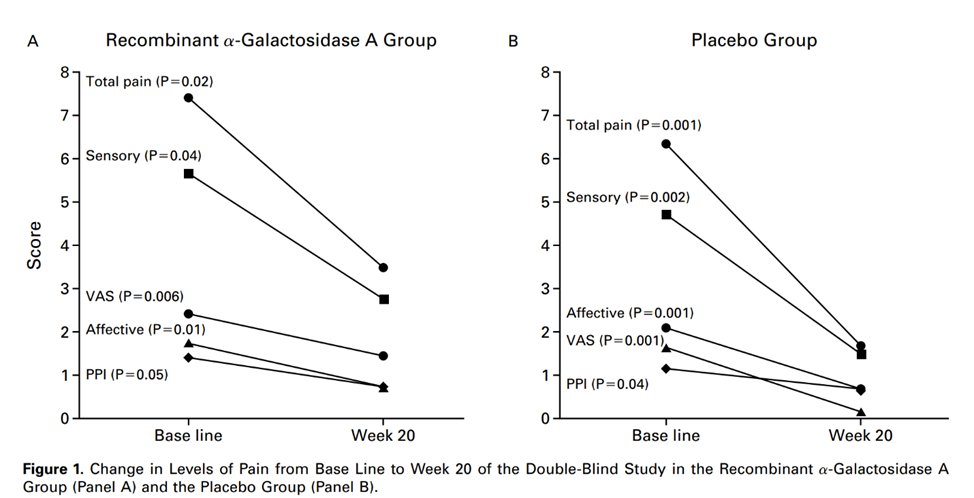
20) In the kidneys, multiple pathways are affected, which result in subclinical proteinuria with progressive CKD if left untreated. Kidney disease occurs in 50% of ♂️ and 20% of ♀️. #NephTwitter
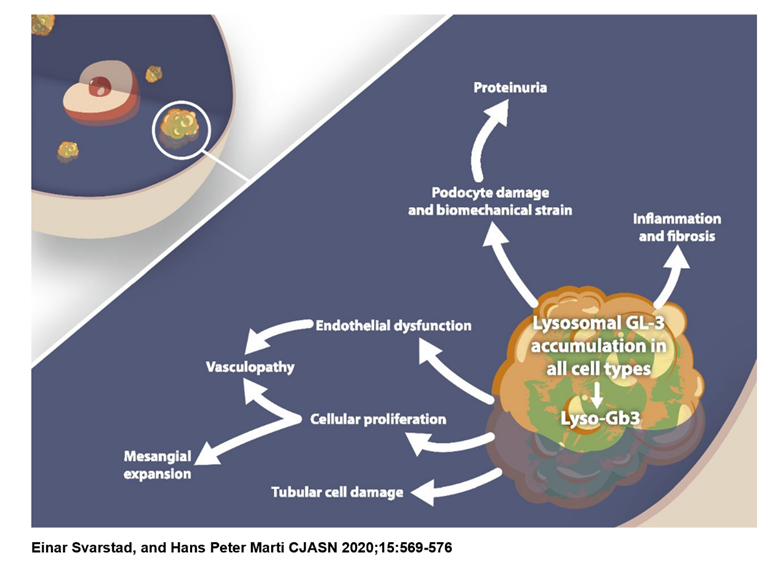
21) #Renal manifestations are variable with the most common one being #proteinuria and progressive #kidneydisease.
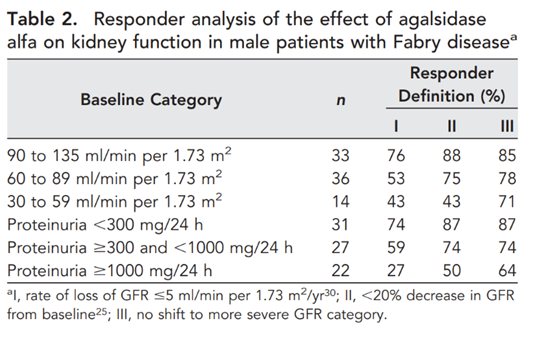
🔓
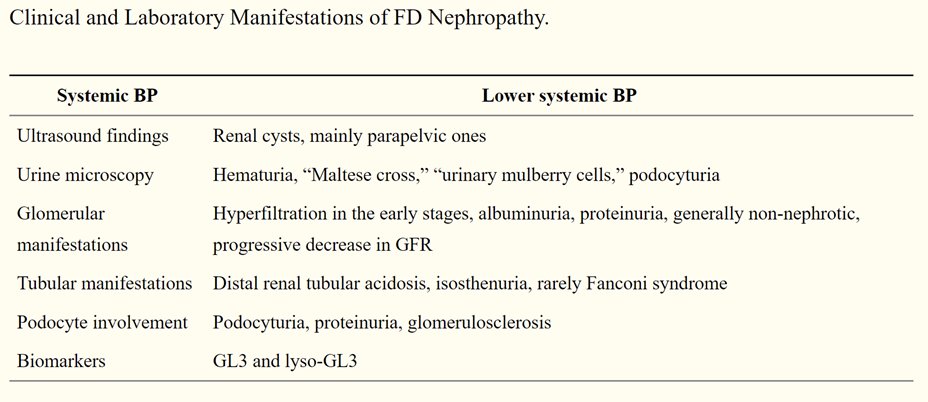
22) Renal biopsy typically shows foamy #podocytes (visceral renal epithelial cells, blue arrows) on light microscopy 🔬and zebra bodies (podocyte myelin figures) on electron microscopy
23) The diagnostic algorithm for FD differs between men and women. Low AGalA level is reliable only in classic early onset disease in men, while women and late onset disease require GLA gene analysis.
24) Endomyocardial biopsy is not usually necessary. Some patients undergoing septal myectomy (1.3% in two reports) are still incidentally diagnosed with #FD.
🔓https://jamanetwork.com/journals/jamacardiology/fullarticle/2647081
🔓
25) Now going back to our case. Amlodipine was substituted with losartan. Ambulatory rhythm monitoring was unrevealing. Patient was counseled about other treatment options. How many FD-specific therapies are commercially available worldwide?
26) The answer is C. Two are enzyme replacement therapies (#ERT) which are Replagal (agalsidase alfa, not FDA approved) and Fabrazyme (agalsidase beta, FDA approved), and one is a chaperone therapy (migalastat).
27) Agalsidase alfa was the first ERT to be investigated. The pivotal study was:
A) RCT w/ improved survival
B) RCT w/ improved neuropathic pain
C) Observational study
D) Mechanism of action
28) Mark your response and return tomorrow for more education on #Fabry disease. And please FOLLOW @cardiomet_CE for regular opportunities all year long to pile up those FREE CE/#CME credits!
Nods to @FabryOrg @FabryDisease1 @Info_Rares @EricWallaceuab1 @renesugar @Ed_Alania
29) Welcome back! You are learning about #Fabry disease & earning CE/#CME credit here on Twitter. Expert author is @MasriAhmadMD. See prior programs still available for credit at http://www.cardiometabolic-ce.com and http://www.ckd-ce.com!
Hi @AAlhatem_MD @HanCardiomd @GiuseppeGalati_
30) Re yesterday's poll (tweet # 27): the answer is B. The first #RCT was performed in the NIH, included classically affected ♂️≥18 years of age. RCT published in 2001. Primary endpoint was reduction in neuropathic pain.
🔓
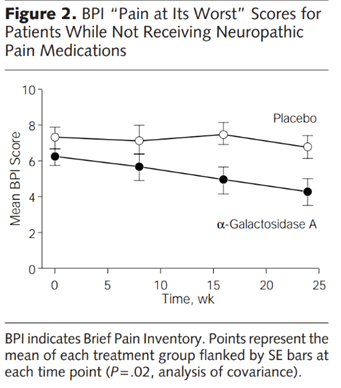
31) The trial also showed decrease in #GB3 compared to placebo and improved #CrCl
32) A subsequent pooled analysis of 108 classically affected males treated with agalsidase alfa did not show a statistically significant difference in GFR decline (-4.8 vs -7).
🔓
33) #GFR decline was less in those with proteinuria < 1g/24 h (i.e. earlier disease).
34) Another RCT of agalsidase beta in 58 patients met its primary endpoint of % of patients in whom renal microvascular endothelial deposits of GB3 were cleared (69% vs 0%).
🔓
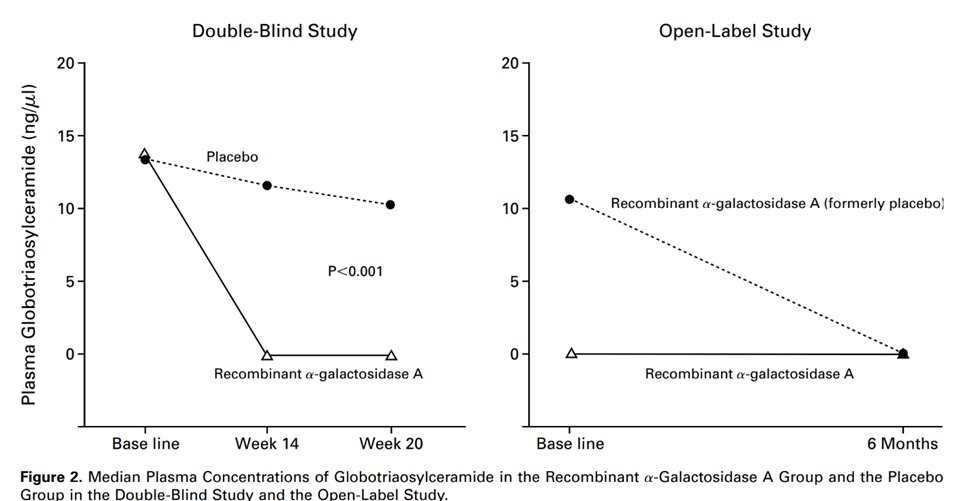
35) However, AGal beta had no effect on kidney function or neuropathic pain
36) In open label follow-up, #kidneydisease progression occurred in 6/58 patients, all >30 y, #proteinuria > 2g/24 h, and had >50% glomerular sclerosis at baseline.
And in the overall population, median #GFR was stable.
37a) In the same study, cont'd clearance of GB3 from different tissues was shown (🔓https://jasn.asnjournals.org/content/18/5/1547.long), & 10-year follow up of that study showed continued efficacy with those younger patients with less kidney involvement benefiting the most (🔓https://jmg.bmj.com/content/jmedgenet/52/5/353.full.pdf).
37b)
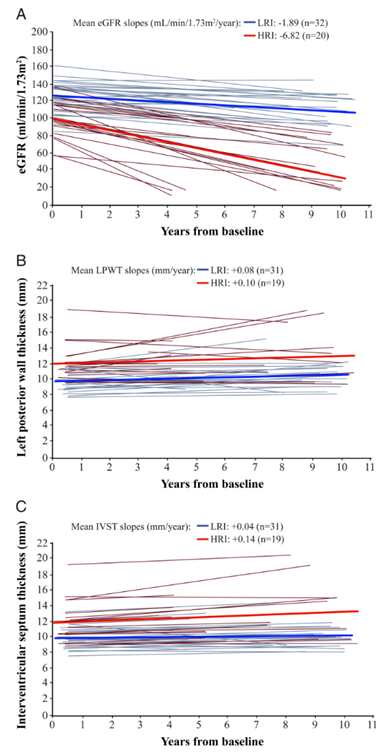
38) Another RCT of agalsidase beta vs placebo in 82 patients with advanced FD showed its efficacy in slowing progression to renal and CV outcomes (27% vs 42%) mainly driven by serum Cr increase > 33%, & confirmed earlier treatment ➡️better outcomes (🔓https://www.acpjournals.org/doi/full/10.7326/0003-4819-146-2-200701160-00148?journalCode=aim).
39) There are no RCTs in ♀️carriers and late onset ♂️disease. Fabrazyme is the only ERT approved by the #FDA (approved in 2003).
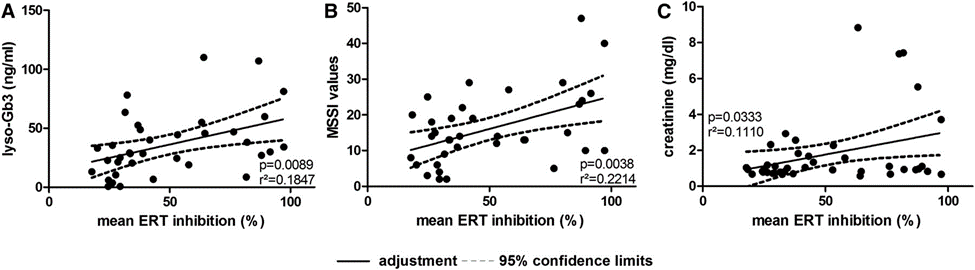
40) Seroconversion w/antibodies vs ERT is very common. Tho initially not thought to affect efficacy of ERT, more studies are showing⬇️efficacy. In 1 study (N=168), ERT antibody (inhibition) was associated w/⬆️GB3 levels & worse disease severity scores.
🔓
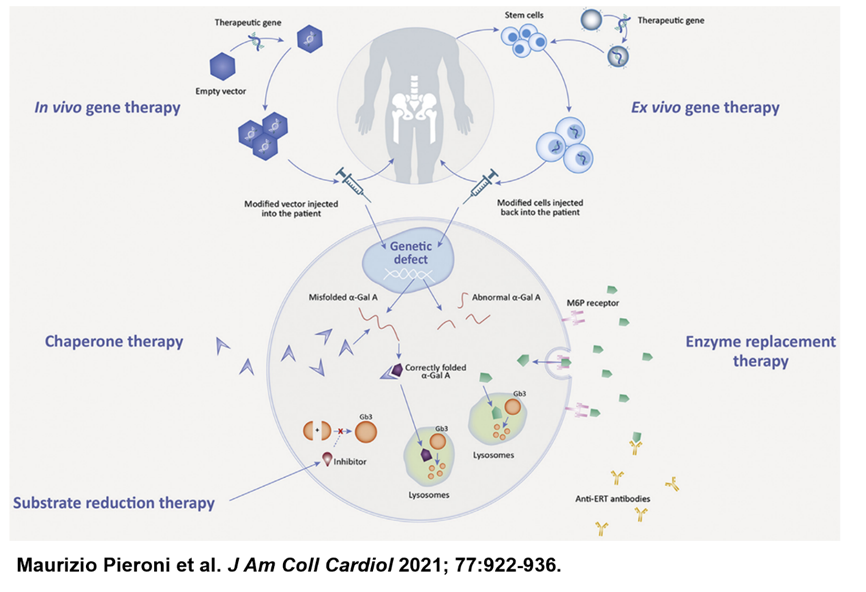
41) The third therapy for Anderson-Fabry is migalastat, which is an oral chaperone therapy that binds AGalA ➡️ trafficking to lysosomes ➡️⬆️d AGalA activity.
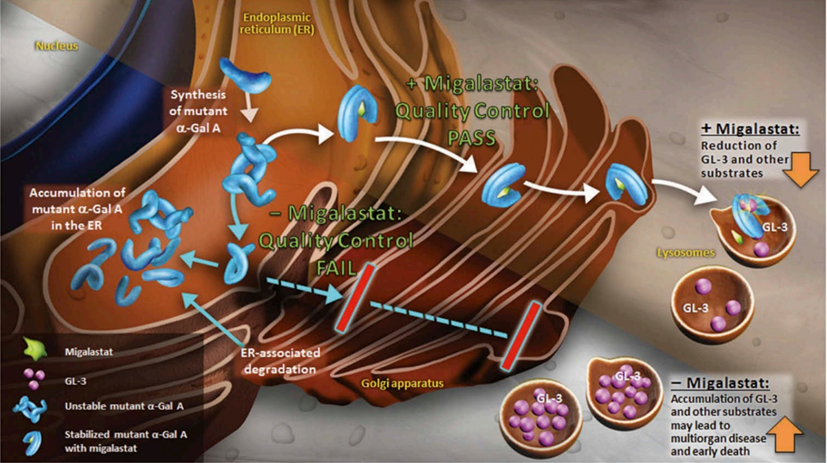
42) Only some mutations/variants are amenable to migalastat. AGalA activity must be < 35% for pts to benefit. https://www.galafoldamenabilitytable.com/reference
In an RCT (n=67; later found 17 didn't have amenable variants), response to migalastat: ≥50%⬇️in # GB3 inclusions/kidney interstitial capillary
43) Response occurred in 41% of migalastat vs 28% in placebo, p=0.30. Combined data (RCT & OLE) showed less #GFR decline and improved #LVH.
🔓
44) Another RCT of patients previously on ERT randomized them to migalastat (n=36) vs ERT (n=21). Comparable effect on renal function at 18 months and improved LV mass.
🔓
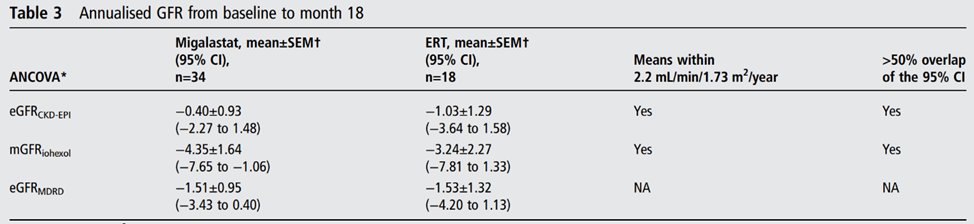
45) FDA approved migalastat in 2018. It remains the only oral therapy for #FD. Monitoring response to therapy is vital since not all biochemically precited amenable mutations respond.
This was shown in real-world data from the FAMOUS study
46) Our patient's mutation was not amenable to migalastat, so Fabrazyme was started 1 mg/kg IV infusion q2wks. The above trials & data show there is significant room for improvement in the care of patients with FD. This is why many therapies are currently under development.
47) Return tomorrow for a wrap-up, some GREAT #casestudies, and a link to your CE/#CME! #cardiotwitter #nephtwitter #cardiomyopathy #FOAMed
Tip o'the hat to @drzgezdentok1 @ecocardio_cl @nephondemand @arh_cardio @MedTweetorials @salvasapedraza @Becho2106 @SmeetaSinha
48) Welcome back! You are just a few🖱️clicks away from FREE CE/#CME while you learn about #Fabry disease and even run through some cases! Expert author is @OHSUCardio's @MasriAhmadMD. FOLLOW US on @cardiomet_CE and @ckd_ce for great education right here on Twitter!
49) The first new therapy under development for #Fabry disease is an improved or second generation #ERT called pegunigalsidase alfa. It is plant based, longer half-life, increased heart and kidney uptake, and low immunogenicity
🔓
50) In a phase 1/2 open-label trial of 18 patients, pegunigalsidase alfa reduced renal peritubular capillary Gb3 inclusions by 84%.
🔓
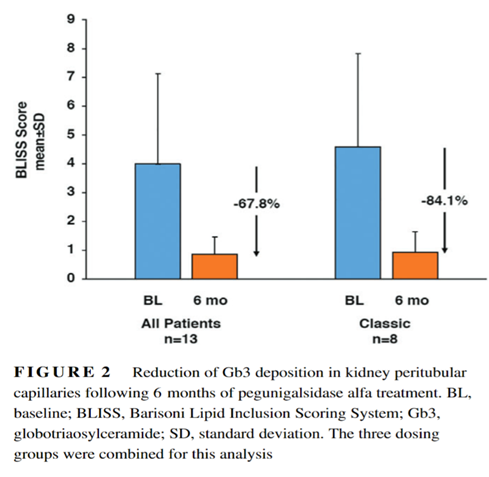
51) The ongoing BRIDGE trial (https://clinicaltrials.gov/ct2/show/NCT03018730) is evaluating pegunigalsidase alfa in 20 patients who switched from agalsidase alfa.

52) Within the limitations of pre-post design, we may expect promising results on kidney function as well as progressive decline in plasma lyso-GB3 and improved immunogenicity.
53) We are awaiting the results of the BALANCE trial (https://clinicaltrials.gov/ct2/show/NCT02795676), a phase 3 trial of 78 patients randomized to pegunigalsidase alfa vs Fabrazyme.
54) Another class in development is substrate reduction therapy, where #iminosugars ➡️inhibit glycosphingolipid synthesis ➡️⬇️GB3. Venglustat (https://clinicaltrials.gov/ct2/show/NCT02228460) & lucerastat (https://clinicaltrials.gov/ct2/show/NCT02930655) are under development. 🔓
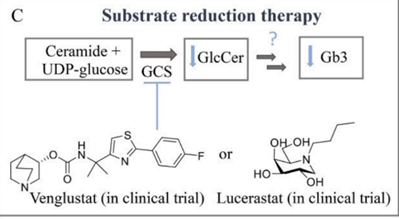
55) While the #mechanismofaction of these oral agents is exciting, a phase III trial (MODIFY, n=182, NCT03425539) of lucerastat vs placebo in #FD failed to reduce neuropathic pain at 6 months. Open label phase ongoing.
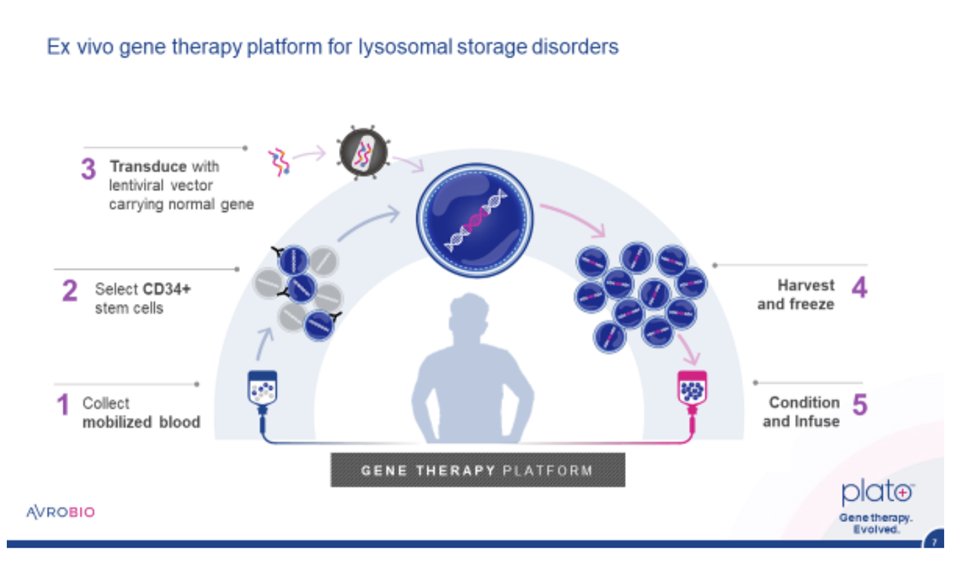
56) Another therapy which was in early phase (NCT03454893) development is AVR-RD-01, an ex-vivo lentiviral gene therapy. However, the sponsor halted the drug development after 5 patients were resistant to engraftment.
57) To summarize: currently 2 FDA approved therapies for #FD: Fabrazyme (ERT) & migalastat (chaperone therapy); a 3rd (Replagal, ERT) is available outside the US. A 4th, pegunigalsidase alfa, is being studied in a phase III trial head-to-head vs Fabrayzme. Results expected 2022
58) We will finish this tweetorial with 3 short cases to encourage everyone to keep #FD on their differential, even if prompted only by the presence of #hypertension. Therapies don’t work if we don’t recognize the disease, especially early in its course.
59) Case 1: 54♂️ who is healthy and exercises daily, had syncope. Echo showed asymmetric #LVH with #LVOT obstruction. CMR done with cines and LGE. Diagnosed with #HCM and given beta blockers.
60) Eventually, 2nd opinion: ICD made repeat CMR w/T1 mapping difficult. Genetic testing ➡️pathogenic variant in GLA gene. No other organs involved. This case illustrates that, while rare, middle aged ♂️ can have FD w/isolated 🫀 involvement.
🔓
61) Case 2: 20♂️ p/w headaches & hypertensive urgency. Found to have severe #LVH & #AKI w/o #proteinuria. Family history of multiple ♂️with sudden cardiac death.
62) While #hypertension is the likely cause, genetic testing was sent to r/o FD. Still, to confirm #LVH is secondary to HTN, strict control of BP was pursued and repeat imaging at 6 months showed significant improvement of #LVH.
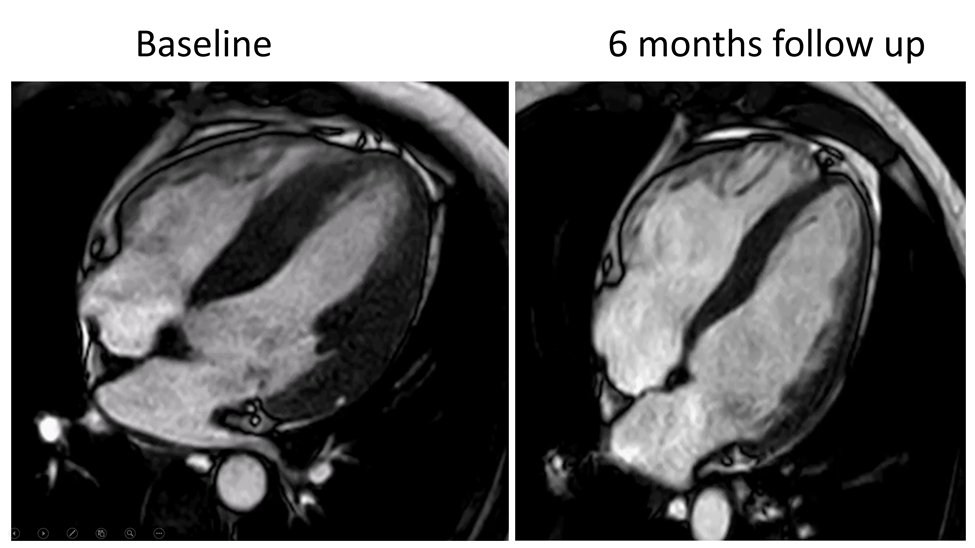
63) Case 3: 57♂️ w/long standing #hypertension, progressive #LVH & #cardiomyopathy, diagnosed with hypertensive heart disease. Presents after a referral related to his ongoing symptoms despite medical therapy.
64) He had #WhyCMR previously, showed severe LVH and severe diffuse enhancement on LGE sparing the subendocardium. T1 mapping was done and was in the mildly abnormal range. Findings thought to be related to HTN.
65) >10 years while under medical care with significant LVH attributed to HTN. #WhyCMR was done with T1 mapping, yet missed the diagnosis of FD due to pseudo/normalization of T1 relaxation time due to fibrosis. 🔓
66) Those cases illustrate that rare diseases will be missed if one does not pay attention to 🚩red flags. #CKD and #LVH (in conjunction or isolation) should not be simply blamed on #hypertension without adequate evaluation. Keep Anderson-#Fabry disease on your mind.
67) And whew–you made it! 0.75h FREE CE/#CME and you are now your group's expert on #Fabry disease! Simply go to http://www.cardiometabolic-ce.com/cardiorenal-Fabry and claim your credit! And please FOLLOW @cardiomet_CE for more education by #tweetorial!
Originally tweeted by cardio-met (@cardiomet_CE) on February 1, 2022.
