1) Welcome to a new #accredited #tweetorial about an important complication of #pulmonaryembolism (#PE): chronic thromboembolic pulmonary hypertension #CTEPH. Follow this thread to earn 0.75h CE/#CME #physicians #physicianassociates #NPs #nurses #pharmacists.
2) I am Jason Weatherald @AlbertaPHdoc of @UAlberta and you may recall my previous tweetorial in this feed. It's still available for credit at https://cardiometabolic-ce.com/pah2/. @cardiomet_CE is your ONLY home for earning CE/#CME entirely on Twitter! Howdy to @vic_tapson @lauralynndonah1

3) This program is intended for #healthcare providers and is supported by educational grants from Actelion, Bayer, Chiesi, & AstraZeneca. Faculty disclosures are listed at https://cardiometabolic-ce.com/disclosures/. Prior programs, still available for credit, are at
4) #PulmonaryEmbolism is common and the 3rd leading cause of cardiovascular death. But there are important long-term complications in those who survive acute PE, including #CTEPH. CTEPH can cause significant morbidity and mortality after #PE. Let’s start with a case!
5) A 67♀️ presents to #emergencymedicine with dyspnea x 3 months that acutely worsens for 3 days. PMHx significant only for #Hypertension. She has taken hydrochlorothiazide for years. She has no prior history of #PulmonaryEmbolism or #DVT.
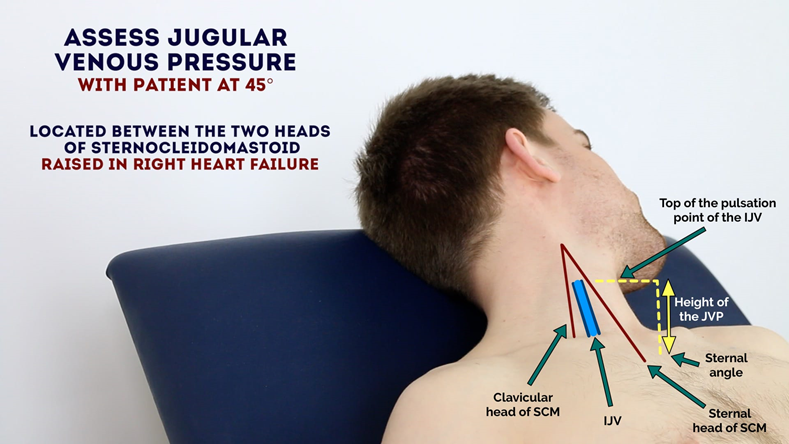
6) On exam: Sats 91% on room air. HR 91, BP 110/75 . Her JVP is elevated at 6cm, there is mild edema. Lungs are clear and there is a parasternal heave. S2 is loud over the right upper sternal border🩺
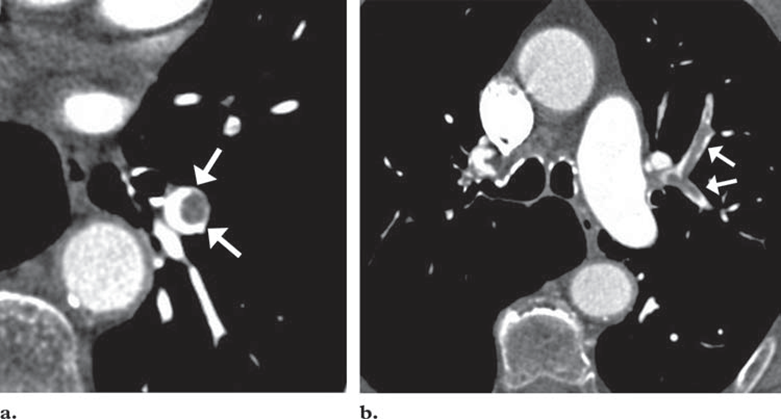
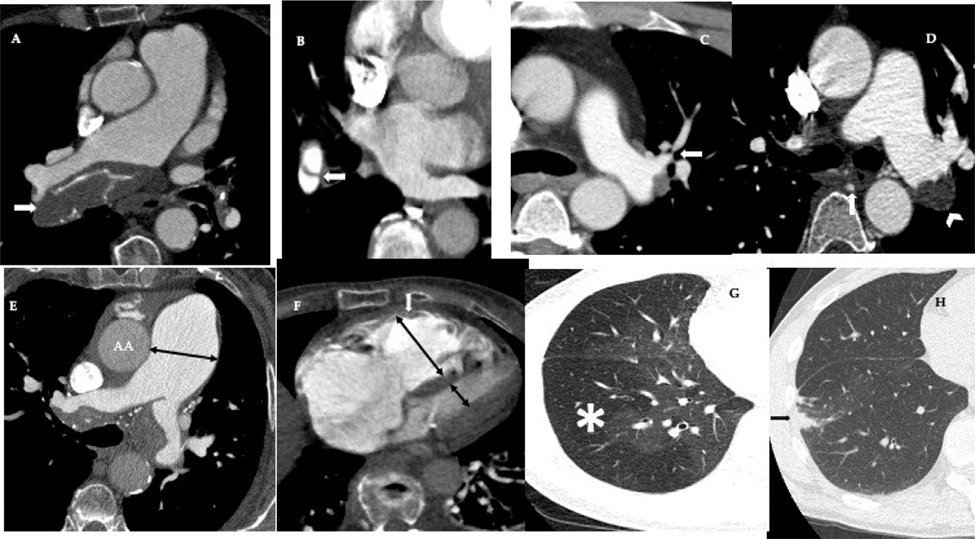
7) Labs: D-dimer ⬆️, NT-proBNP⬆️at 2000 ng/L, T-wave inversion in V1-V6. A #CT pulmonary angio is done. See images below:
8) What do you see? There are bilateral filling defects in the proximal pulmonary arteries consistent with pulmonary embolism, but they have a “chronic” appearance to them. Geez, if only these scans always came with the red arrows!
9) Clot from acute PE tends to more central, similar to a “bulls-eye":
Acute #PE, from 🔓
10) CTEPH occurs from incomplete resolution and fibrotic organization of thrombus leading to vascular obstruction. See 🔓
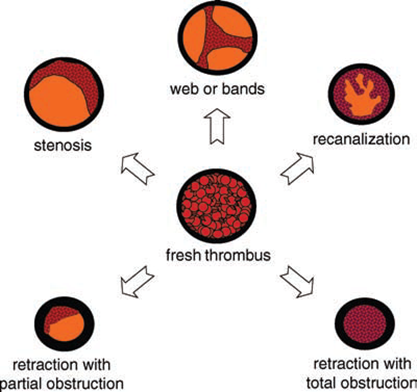
11) Other CT features of #CTEPH include webs, bands, complete occlusions & focal stenoses. Calcification of thrombus ➡️ chronicity. Dilation of the pulmonary artery & RV & heterogenous attenuation of the lung (mosaic attenuation) are also often present 🔓
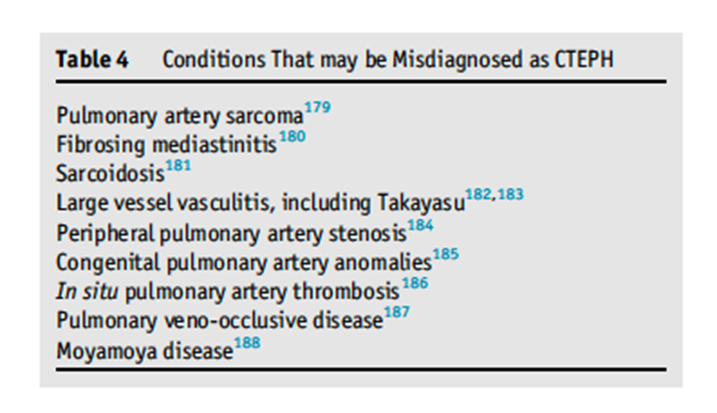
12) For the #radiology buffs and those who like long lists of #ddx, there are several conditions that can mimic #CTEPH on imaging. 🔓https://doi.org/10.1016/j.healun.2021.07.020
And, for adding consideration of #moyamoya disease to your day . . . YOU ARE WELCOME
13) Time for a brief #Inception thread: A 🧵 within a 🧵! Why is it important to know about & recognize CTEPH? Here are3⃣ good reasons:
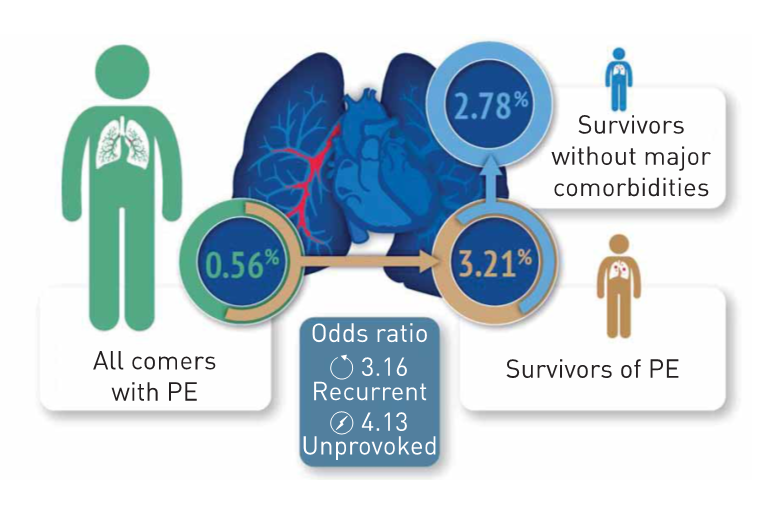
1⃣ CTEPH is not that rare! #PE is common. CTEPH occurs in ~ 1/30 or 3% of survivors of acute PE! (fig from 🔓https://erj.ersjournals.com/content/49/2/1601792.long)
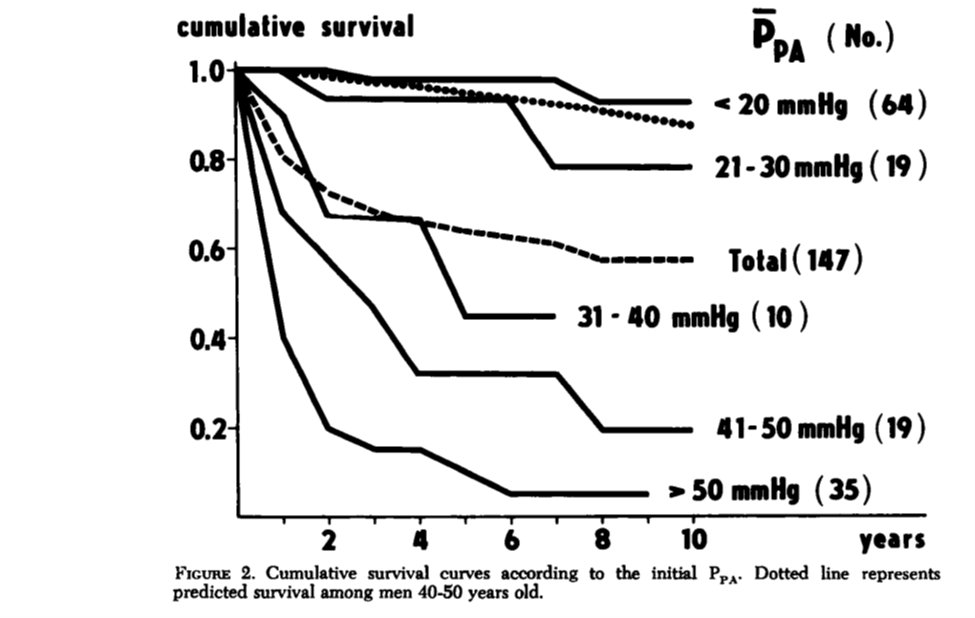
14) 2⃣ Untreated, #CTEPH carries a 70% mortality by 5 years! #CTEPH leads to progressive [Up arrow] in pulmonary pressure, dilation & failure of the #RightVentricle. Higher pressure = worse outcomes.
See
15) 3⃣ The most important reason to think about (and find) CTEPH is that effective treatments (and often a cure) exists…more on that later.
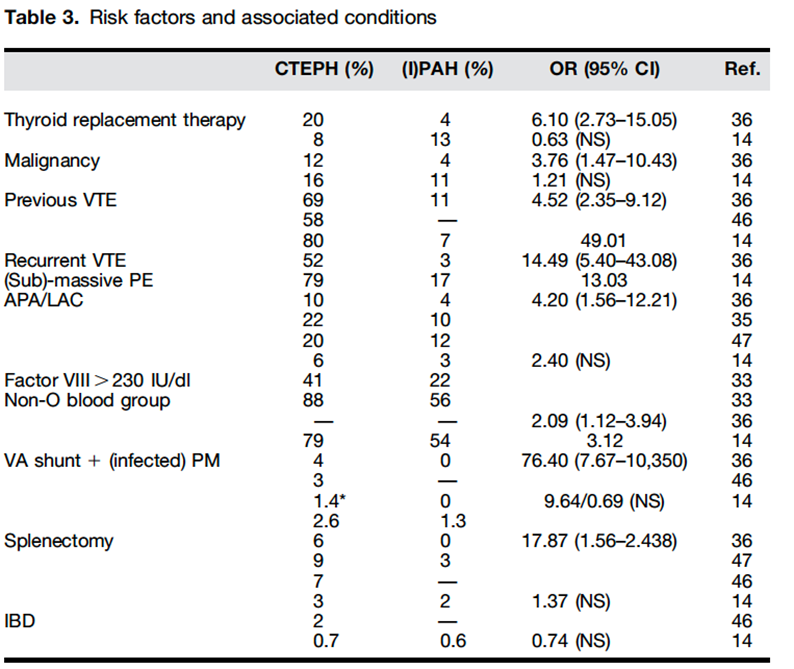
16) There are several well recognized risk factors for developing #CTEPH including ⬆️Factor VIII, #antiphospholipid antibodies, #splenectomy, #IBD and infected shunts. See 🔓
17) Back to our patient in the ED. She has signs of chronic PE and pulmonary hypertension on imaging & is hemodynamically stable. What is the most appropriate initial management?
A. Anticoagulation x 3 months
B. Thrombolysis
C. Catheter-directed thrombolysis
D. Thrombectomy
18) Mark your best answer and return tomorrow for MORE education & MORE on this case. Don't miss it!
@kurt_prins @PGeorgeMD @anjalivaidyaMD @rjbernardoMD @SashaPrisco @mdlizs @LucillaPiccari @3CPRCouncil @MakLab_
19) Welcome back! We are learning ALL about #CTEPH from expert author #pulmonologist #PH specialist @AlbertaPHdoc. And YOU have found the ONLY source for #serialized #tweetorials that bring CE/#CME credit!
@SandeepSahayMD @EstefaniaOS @ISHLT @PHAssociation @Erik_Klok_MD
20) Yesterday's quiz? Scroll back⤴️to 17 if you didn't answer!
A. Anticoagulation for 3mos is best initial management. Diagnosing #CTEPH requires 1⃣ at least 3mos of effective anticoagulation 2⃣Pulmonary hypertension 3⃣Persistent obstruction on imaging. 🔓
21) Our patient in the ED likely has #CTEPH, given CT feature & symptom chronicity. In some cases, adequate course of anticoag can improve burden of thromboembolic disease. Close follow-up is required & patients who worsen or have right heart failure need urgent, definitive Rx.
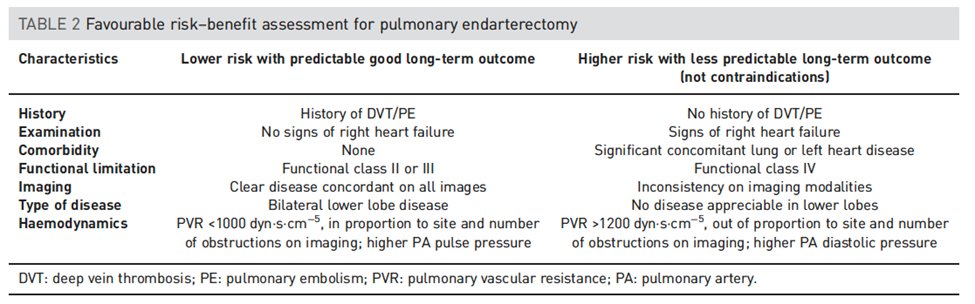
22) Side note: it is always important to consider #CTEPH in a patient with #pulmonaryhypertension. Importantly, NOT all patients with CTEPH have prior history of #VTE. In a patient with #PH on #Echocardiogram, what is the best screening test to rule out #CTEPH? VOTE before ⤵️!
23) Answer: A. Ventilation/perfusion is recommended first to rule out CTEPH. See the diagnostic algorithm below from the @EuroRespSoc 🔓
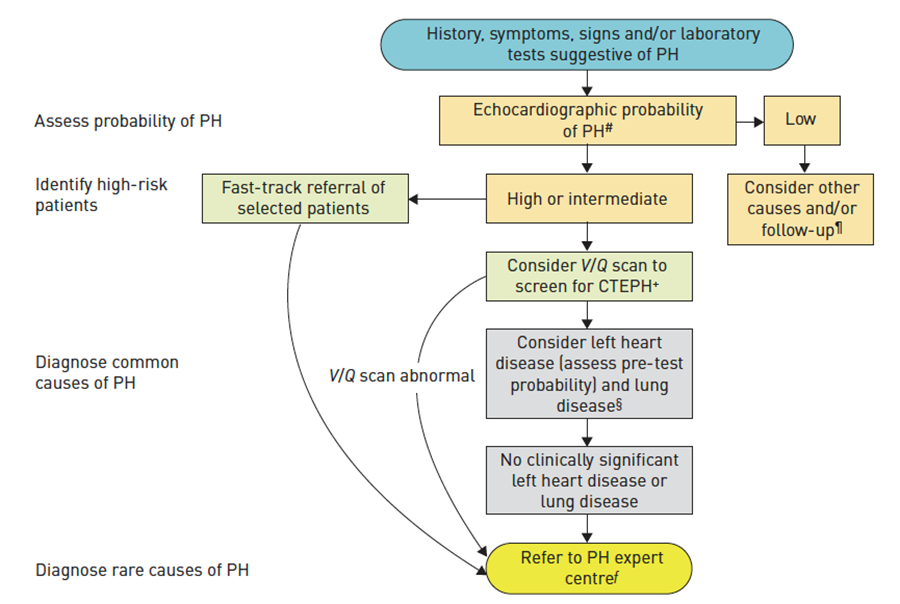
24) In the #PulmonaryHypertension diagnosis algorithm, VQ comes first, as the sensitivity is higher than CT. A normal VQ effectively rules out CTEPH.
25) Defects on VQ (top) suggests CTEPH but can’t differentiate acute from chronic clot. VQ-SPECT CT (bottom) improves Specificity by visualizing areas of parenchymal lung disease
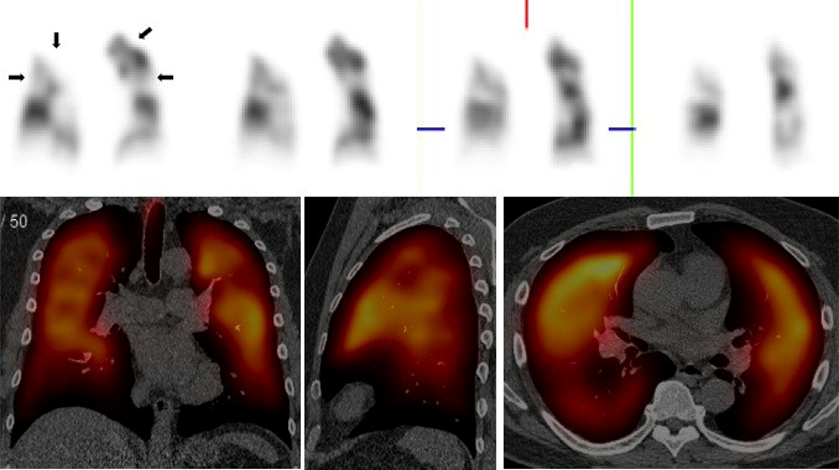
26) If the VQ is abnormal, the next step should be a CT pulmonary angiogram to confirm the presence of #CTEPH and to determine whether it is surgically operable.
27) Pulmonary #thromboendarterectomy (PTE) is the treatment of choice for #CTEPH patients who are candidates for surgery. All patients require lifelong #anticoagulation and evaluation for PTE. 🔓
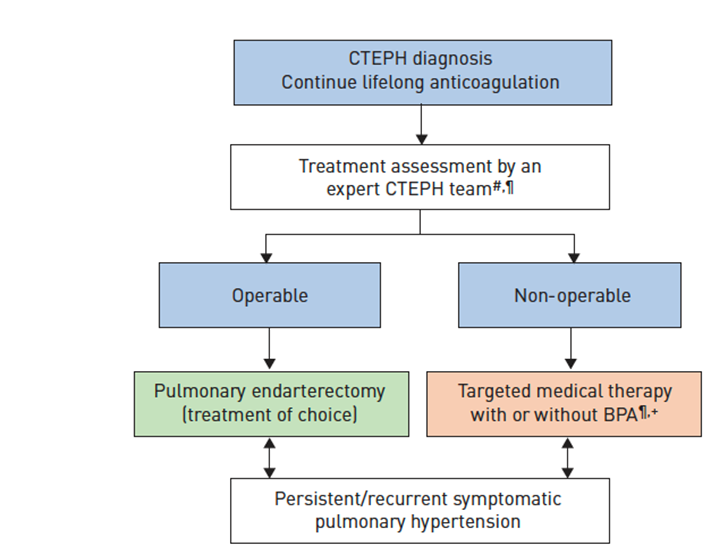
28) PTE involves a sternotomy and cardiopulmonary bypass. Patients undergo deep hypothermia to protect neurologic function as the removal of thromboembolic material is done under full circulatory arrest. See 🔓
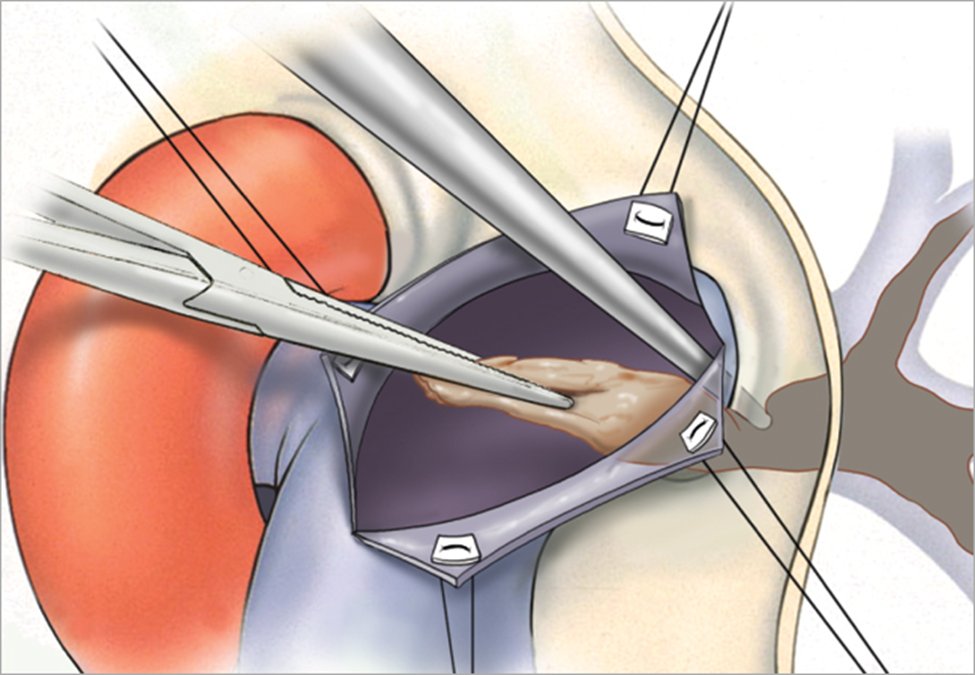
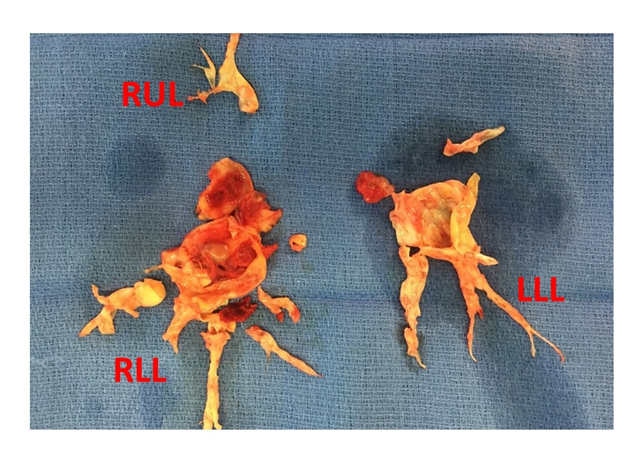
29) Once the thromboembolic material is removed, the pulmonary vascular resistance and pulmonary artery pressure are usually markedly lower and recovery can begin. An example of surgical specimen from PTE is below.
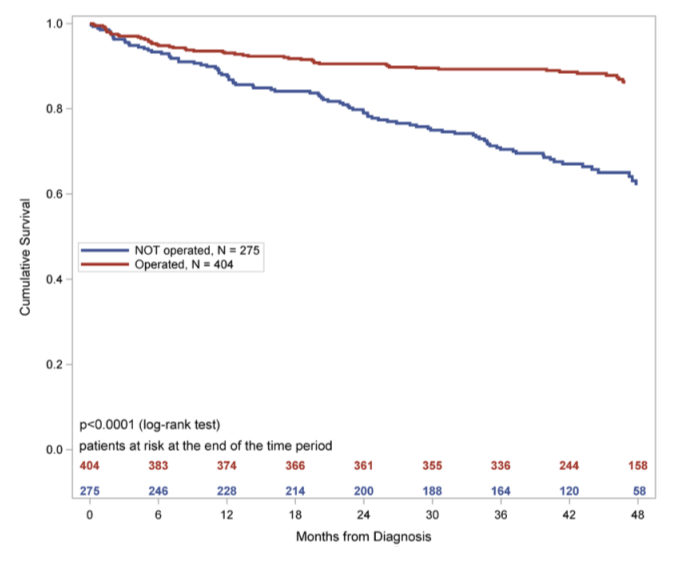
30) For patients able to successfully undergo PTE surgery, long-term survival is markedly better with >90% survival at 5-years. 🔓
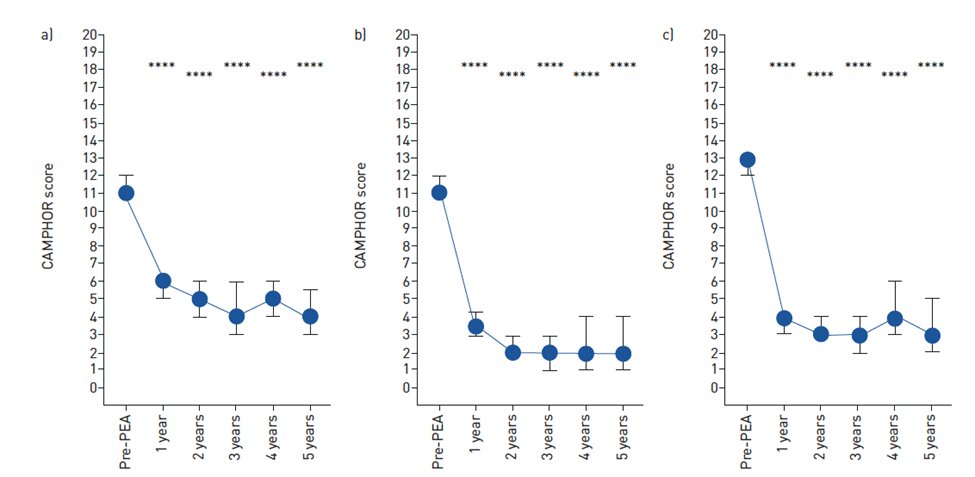
31) Exercise capacity, quality of life and symptoms are also markedly improved after PTE. This figure shows rapid improvements in the #CAMPHOR questionnaire for a) activity b) quality of life and c) symptoms
32) PTE is major surgery that carries risks, but it's also potentially curative. Determining whether a patient is a good candidate for PTE req's multidisciplinary discussion in an expert #CTEPH surgical centre. Factors related to surgical suitability:🔓
33) So for patients unable or unwilling to undergo PTE surgery, which other treatment options can be considered?
A. Balloon pulmonary angioplasty (BPA)
B. Riociguat
C. Lung transplantation
D. All of the above
34) Mark your best answer and RETURN TOMORROW for a wrap-up of this program & your certificate for 0.75h 🆓CE/#CME 🇺🇸🇬🇧🇪🇺🇨🇦!
@CTEPHAdvisor @PVRI @heresi_gustavo @RogerAlvarezDO @LaurentBertole1 @SaraHegabMD @PForfiaPHDOC @ebrosenzweig @DocAsger @DocHirsch @ICA_CTEPH @madelcroix
35) Welcome back! You are just a few 🖱️clicks away from 0.75h CE/#CME! And what a ride! @AlbertaPHdoc is teaching us ALL about #CTEPH–a big problem! Per 🔓https://pubmed.ncbi.nlm.nih.gov/28356407/, incidence of CTEPH in 🇫🇷🇩🇪🇮🇹🇪🇸🇬🇧🇺🇸🇯🇵 is dramatically ⤴️ing, as is severity at the time of dx.
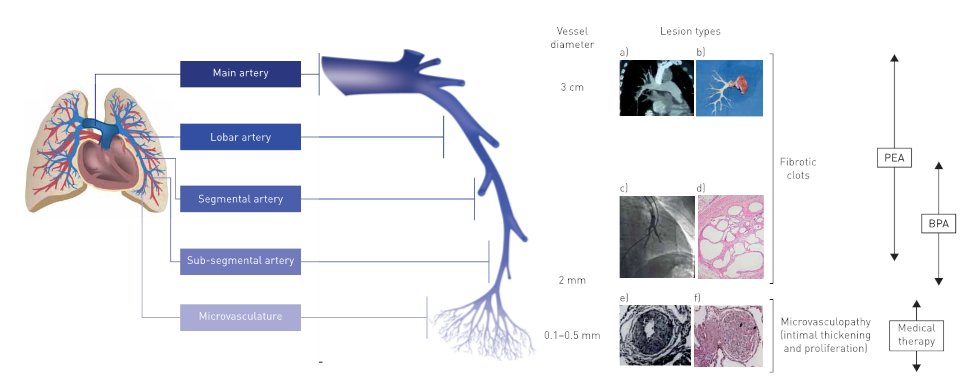
36) Yesterday's quiz (tweet 33) answer is D. Some pts have distal disease in subsegmental vessels or in the pulmonary microcirculation that is inaccessible to surgery. Some are medically unable to undergo PTE due to comorbidities.
37) #Riociguat and/or #BPA are both options in such patients. Lung Tx can be considered in those with refractory #PH after medical Rx or BPA.
38) The choice of medical therapy with riociguat or BPA depends on the location of the #CTEPH lesions. Some patients receive a combination of PTE (a.k.a. PEA), BPA and medical therapy. 🔓
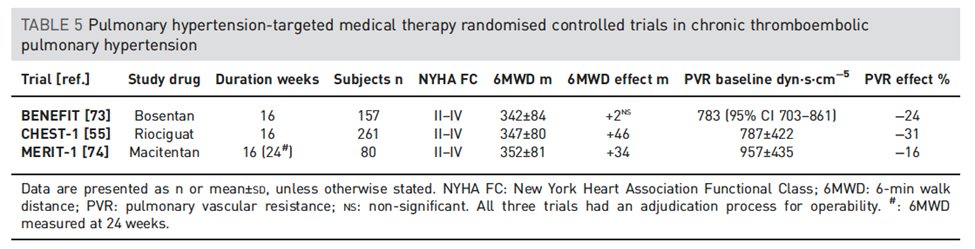
39) Currently #riociguat is the only medical therapy approved by the @US_FDA for #CTEPH. Other studies tested #bosentan and #macitentan, but they are not approved (both are endothelin receptor antagonists used in pulmonary arterial hypertension). 🔓
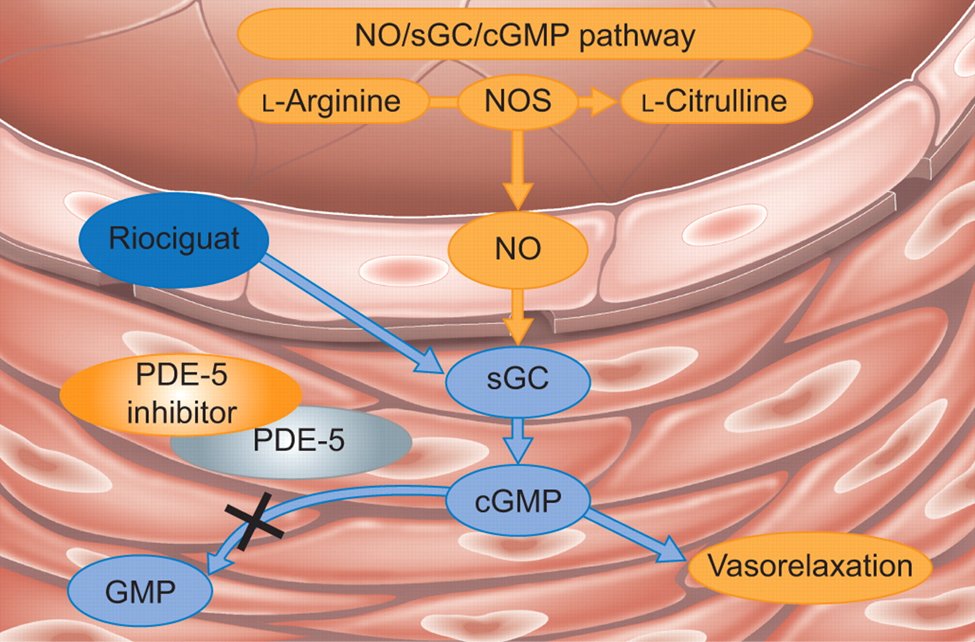
40) Riociguat is a soluble guanylate cyclase stimulator that increases #cGMP in pulmonary arteries leading to vasodilation and lower pulmonary vascular resistance. It acts independently of nitric oxide availability 🔓
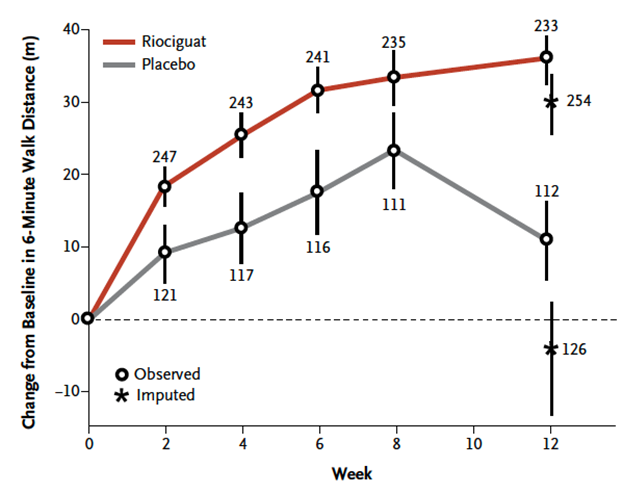
41) In the CHEST-1 trial, riociguat improved 6-minute walking distance by 36 meters (36 m; 95% CI, 20 to 52 m) at 12 weeks vs placebo, which led to its approval for #CTEPH. See 🔓
42) The phase 2 MERIT-1 trial compared #macitentan to placebo for inoperable #CTEPH and demonstrated a ⬇️ in pulmonary vascular resistance #PVR of 26% and ⬆️ #6MWD by 34m at 24 weeks 🔓
43) #BPA is a catheter-based approach like coronary angioplasty where a wire crosses a #CTEPH lesion in a small segmental or subsegmental artery. A balloon is inflated to dilate and disrupt the obstructing lesion and improve blood flow.
🔓
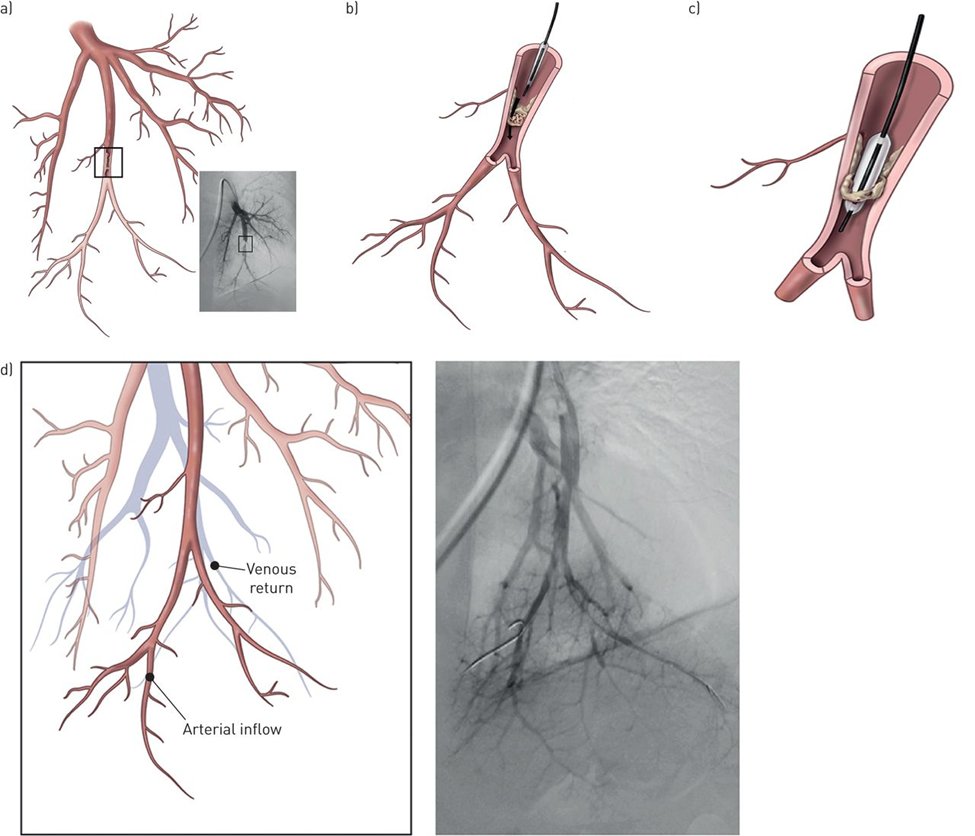
44) Here is a video of a lower lobe BPA procedure with sluggish, minimal blood flow before ballooning and markedly improved blood flow afterwards.
45) Exercise intolerance in #CTEPH is multifactorial & other defects in the oxygen delivery and uptake pathway may contribute to impairment. Even after restoring or improving cardiac function, many patients have residual peripheral muscle dysfunction 🔓
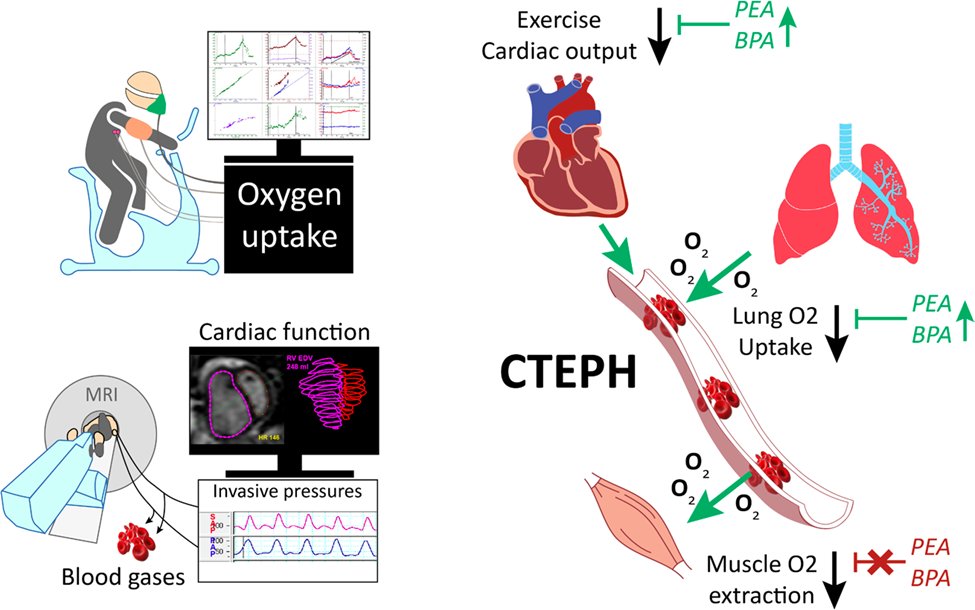
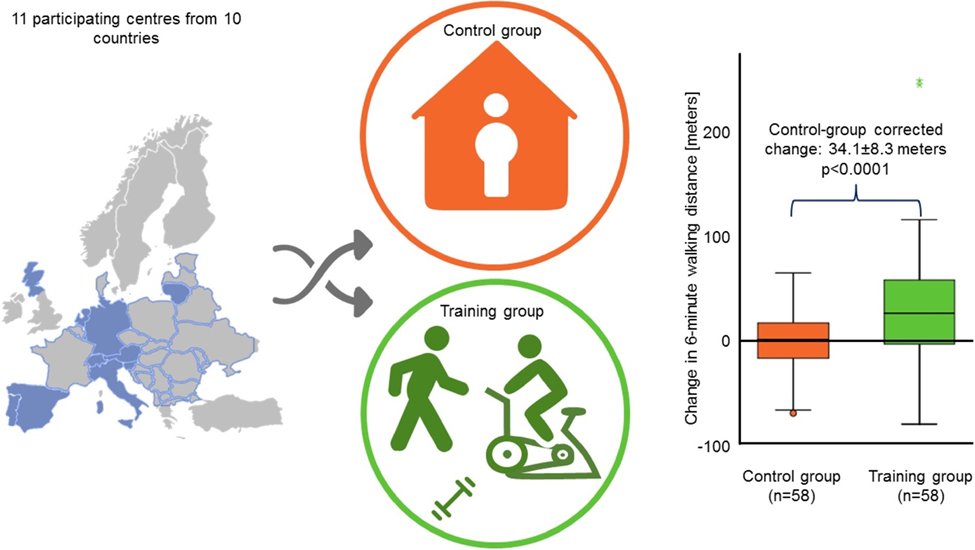
46) These residual peripheral factors in #CTEPH highlight the role of #exercise training & #rehabilitation. Indeed, a recent RCT of exercise training showed improvements in exercise capacity as is seen with adding medical therapy!
47) There you go! In summary, #CTEPH is an important complication of #VTE but many patients have no prior history of #PE or #DVT. Always consider #CTEPH in a patient with #pulmonaryhypertension
48) Management of #CTEPH includes careful evaluation for #PulmonaryEndarterectomy, lifelong anticoagulation, #BalloonPulmonaryAngioplasty, #riociguat and #exercise training.
49) And now go grab your #CME/CE certificate. You earned it! It's at https://cardiometabolic-ce.com/pah3/. FOLLOW US and EARN MORE!! I am @AlbertaPHdoc. Tip o' the hat to @SarahMedrek @HelpMyBreathing @mark_toshner @SudarRajagopal @3CPRCouncil @ATS_PC
Originally tweeted by cardio-met (@cardiomet_CE) on April 12, 2022.
