1) Welcome to an #accredited #tweetorial on aggressive treatment of elevated #LDL-C in the post-MI and/or #diabetic patient to improve #ASCVD outcomes. Our returning @cardiomet_CE expert author is cardiologist Christopher Cannon MD @cpcannon of @harvardmed & @BrighamWomens.
2) This #tweetorial, accredited for #CME/CE and intended for #physicians #physicianassociates #nurses #nursepractitioners #pharmacists is supported by an educational grant from Esperion Therapeutics. See faculty disclosures at https://cardiometabolic-ce.com/disclosures/.
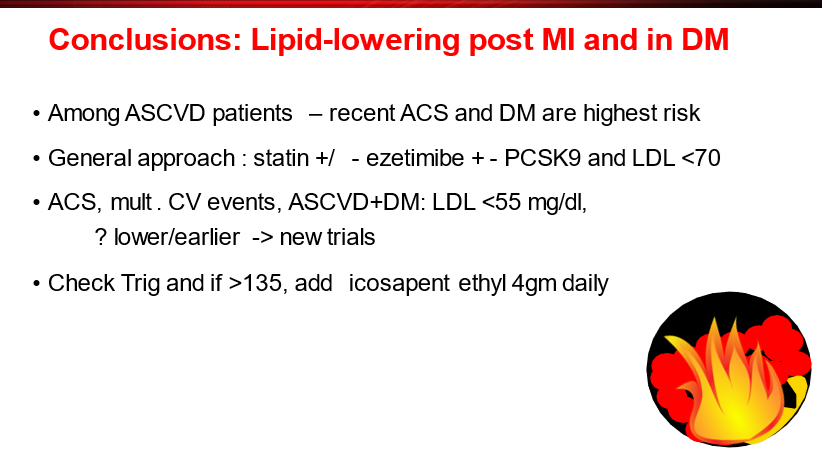
3) We tackle here a population with #ASCVD at very high risk for #CV morbidity and mortality. This is SECONDARY prevention and it involves a multimodal approach including #lifestyle modification and lipid-lowering therapy #LLT to⬇️#LDL-C.
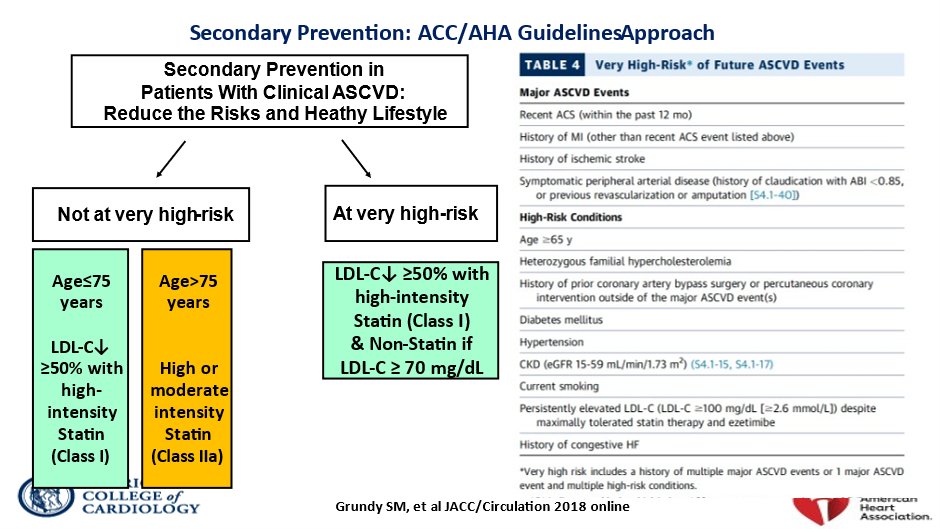
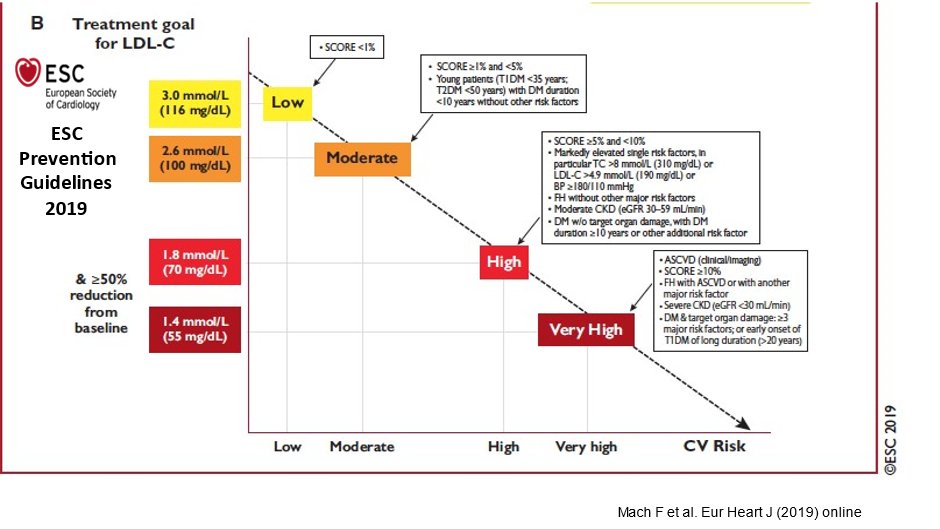
4) The ESC guidelines nicely illustrate that treatment goals for high-risk #ASCVD patients should be titrated to that risk
🔓
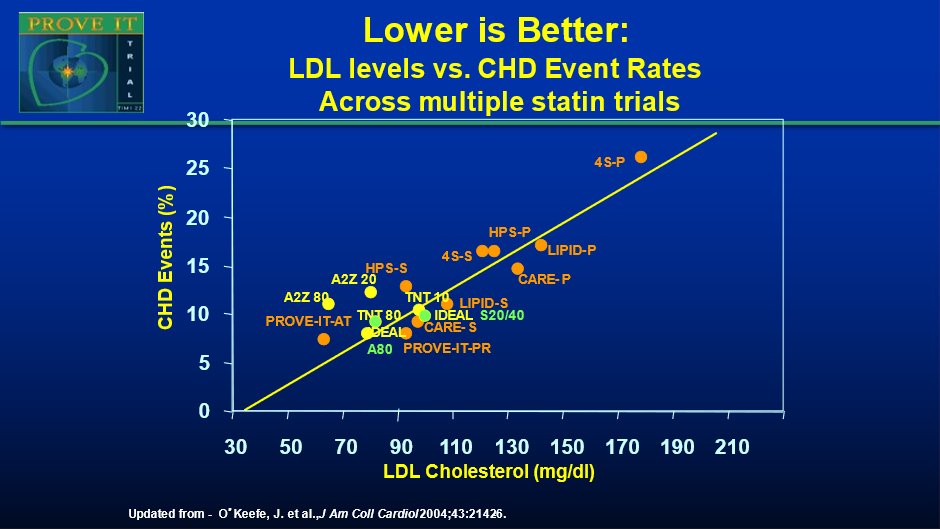
5) As shown in this plot of CV event rates across many trials: as achieved LDL goes down, so do CV event rates. As such “Lower is better” emerged as a mantra (that holds up!)
6) To achieve sufficiently dramatic reductions in #LDL-C in these high-risk patients, investigators have turned to combinations of agents and to later novel mechanisms such as #monoclonal antibodies and #RNA editing
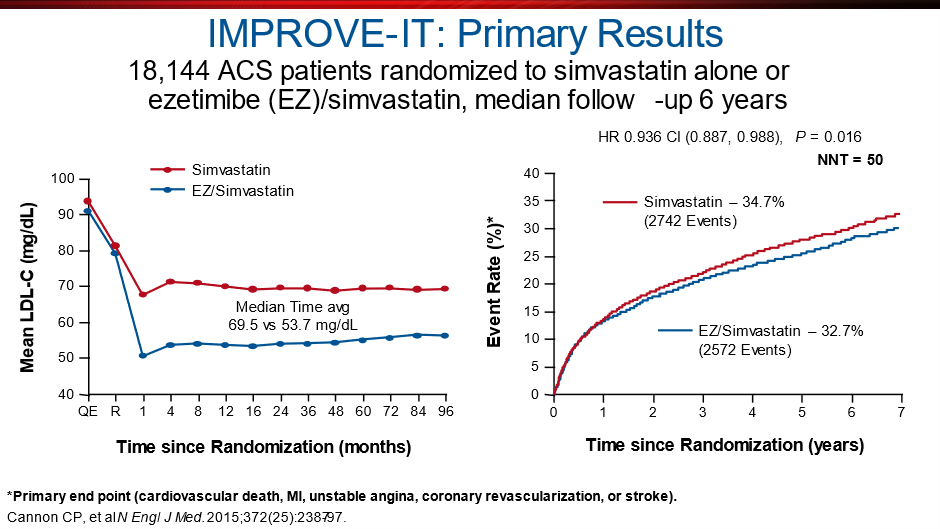
7) A large trial of combination therapy for CV event reduction was IMPROVE-IT (🔓https://www.nejm.org/doi/full/10.1056/nejmoa1410489) compared statin alone vs. statin+ #ezetimibe. Primary end point was a composite of #CV death, nonfatal #MI, unstable angina, or coronary revasc.
8) Eligible pts had been hospitalized for #ACS within past 10d & had LDL-C of 50-100 if already on #LLT or 50-125 if not. Clearly a high-risk population! Median follow-up was 6 years.
9) Results ➡️when added to statin therapy, #ezetimibe resulted in incremental lowering of #LDL cholesterol levels & improved #cardiovascular outcomes. The data also supported the "lower is better" thesis: ⬇️ing LDL-C to below previous targets provided additional benefit.
10) Another option for combo therapy, even on top of ezetimibe+statins for battling established #ASCVD is #bempedoic acid. (BTW, see the excellent #tweetorial, still available for credit, by @PaulDThompsonMD on the MOAs of ezetimibe & bempedoic acid, at https://cardiometabolic-ce.com/lipids3/.)
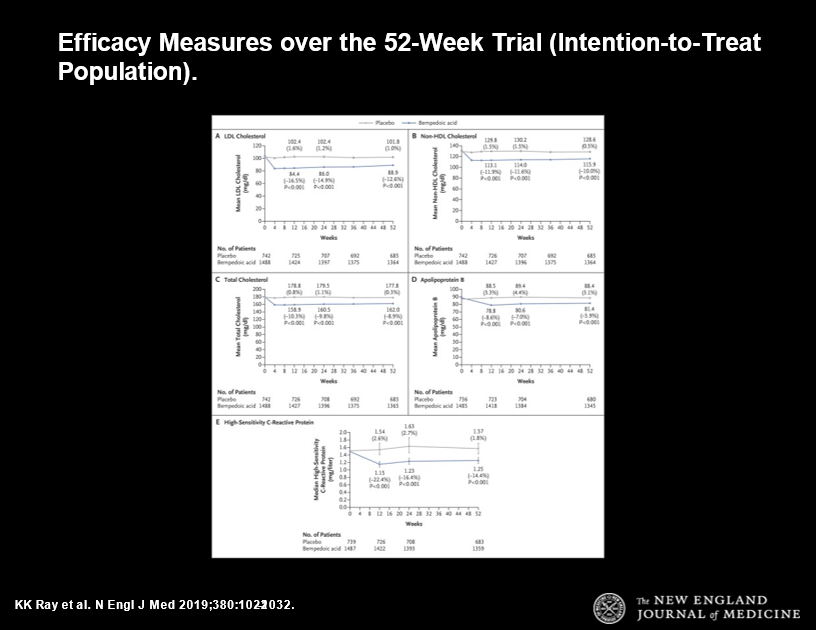
11a) Phase 3 trials of bempedoic acid: CLEAR-HARMONY 1 yr placebo-cont RCT of 2230 pts with ASCVD, heterozygous familial hypercholesterolemia #HeFH or both. Patients had to be receiving maximally tolerated statin therapy with an LDL-C level of at least 70 mg/dL.
11b) Bempedoic acid ⬇️#LDL-C levels by 16.5% > placebo and had no diff in AEs, including no increase in muscle symptoms. 🔓https://pubmed.ncbi.nlm.nih.gov/30865796/, led by @cardiomet_CE faculty @ProfKausikRay
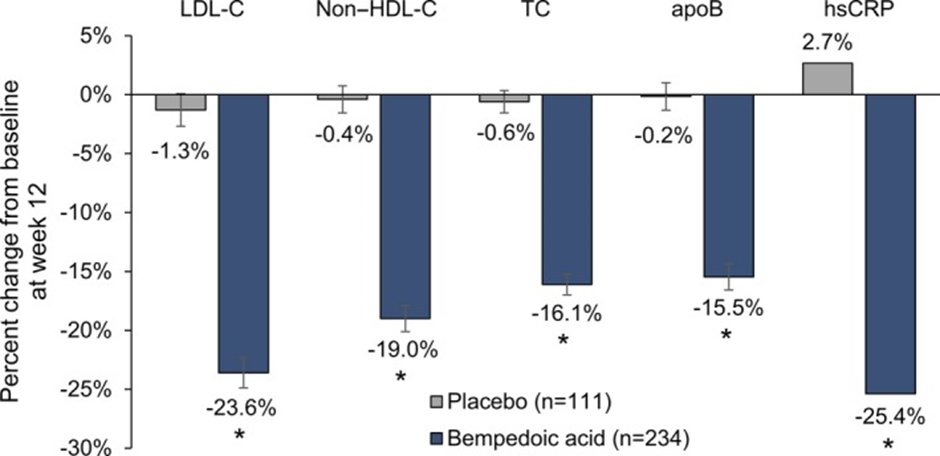
12a) On to CLEAR-SERENITY: 24 wk placebo-cont #RCT 345 pts w/ hypercholesterolemia + history of intolerance to at least 2statins w/ 1 at the lowest available dose. At 12wk, bempedoic acid arm ➡️23.6% reduction in #LDL-C levels vs 1.3% ⬇️ for placebo (p<0.001).
12b) This study confirmed utility of bempedoic acid in pts w/statin intolerance. 🔓
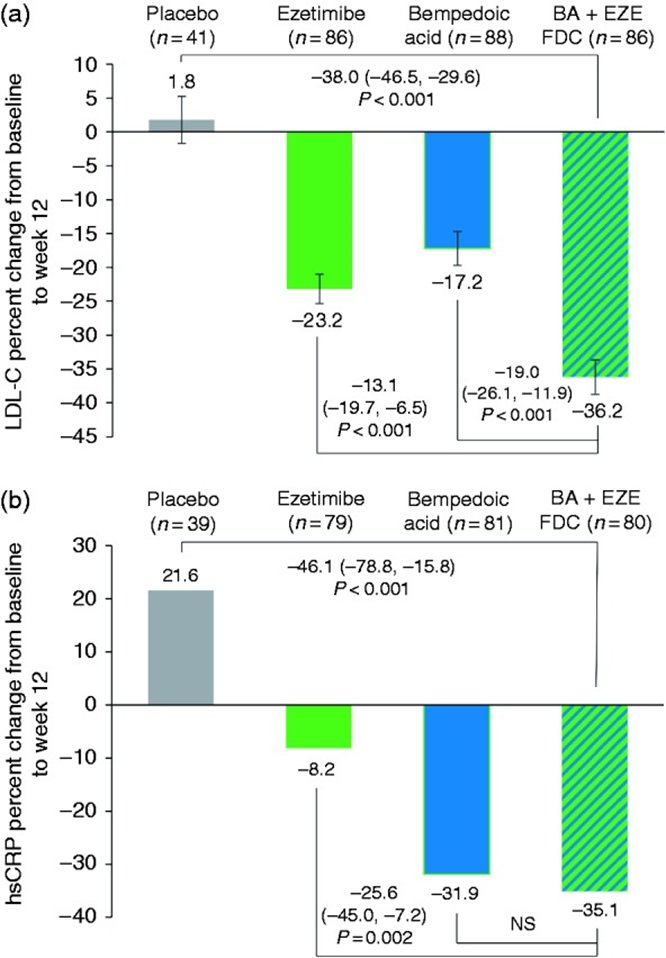
13a) CLEAR-TRANQUILITY (🔓https://pubmed.ncbi.nlm.nih.gov/29910030/) led by @cardiomet_CE author @CBallantyneMD, confirmed those findings, and then he went on to demonstrate the safety & of the #ezetimibe+bempedoic acid combo in 301 pts w/ established #ASCVD, #HeFH, or multiple #CV risk factors.
13b) That was 🔓https://pubmed.ncbi.nlm.nih.gov/31357887/ and at 12ek, w/no safety issues, combo ➡️36.2% ⬇️ in LDL-C levels vs 17.2% ⬇️ w/ bempedoic acid vs. 23.2% ⬇️w/ezetimibe arm, vs. 1.0% ⬆️ in the placebo treatment arm.
14) So what about #monoclonal antibodies for patients with ⬆️⬆️#LDL-C in the post-MI patient? There are fully human monoclonal antibodies that inhibit proprotein convertase subtilisin/kexin type 9 #PCSK9.
15) #PCSK9 inhibitors work by preventing destruction of LDL receptors in the liver, thereby allowing LDL receptors to remove many more LDL-C particles, and lower LDL-C by 55-60%
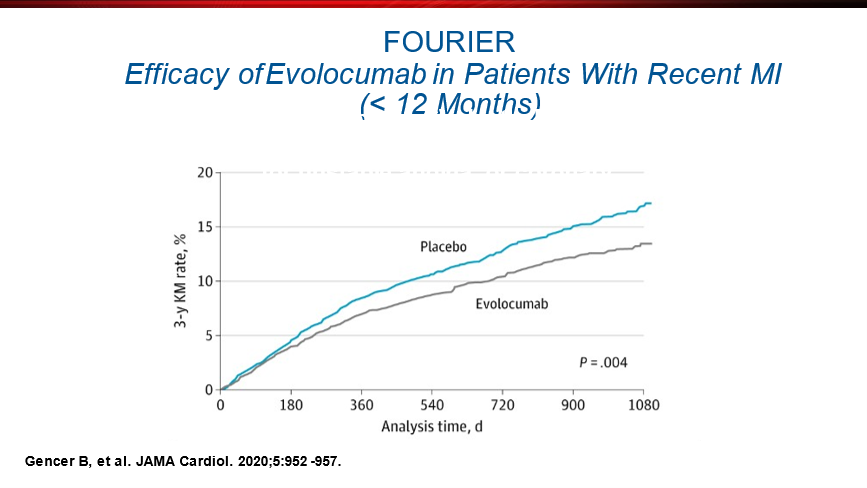
16) In a prespecified secondary analysis from the #FOURIER trial in subgroup of 5711 pts with a recent MI, #evolocumab significantly ⬇️risk of comp outcome of #CV death, #MI, #stroke, #unstableangina, or coronary revasc by 19%; NNT=27 over 3y. 🔓
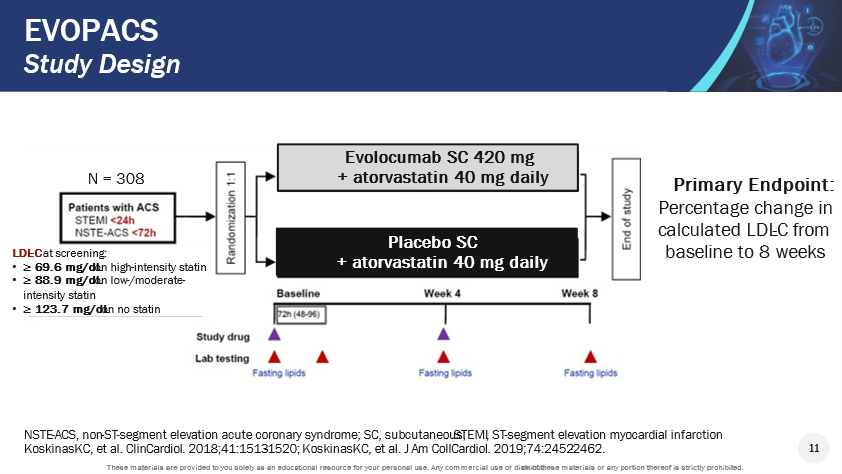
17) #EVOPACS aimed to address the fact that although guidelines rec in-hospital initiation of high-intensity statin therapy in pts with #ACS, #LDL-C target levels are frequently not attained. The🔓https://pubmed.ncbi.nlm.nih.gov/31479722/ #RCT eval'd 308 pts w/ #ACS & ⬆️LDL-C despite #statins.
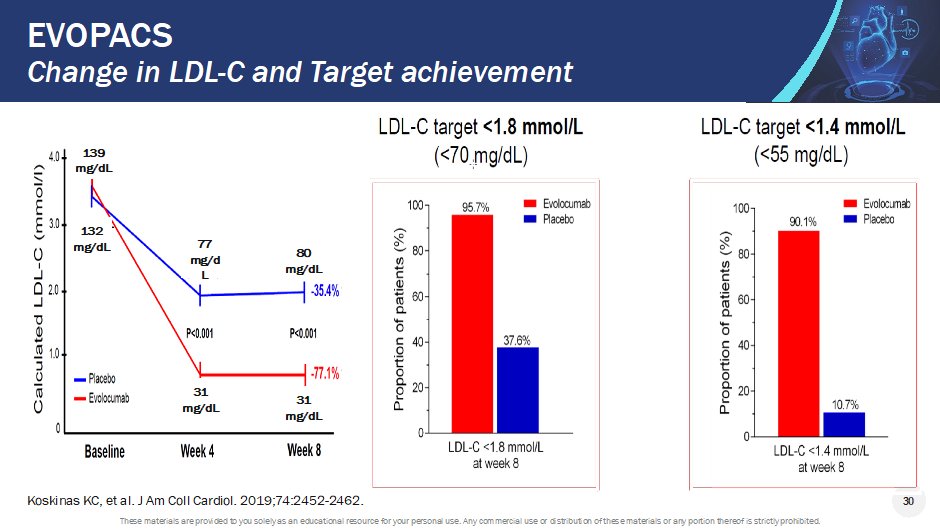
18) LDL-C levels <1.8 mmol/l were achieved at week 8 by 95.7% of pts in the evolocumab group vs 37.6% in the placebo group. Adverse events and centrally adjudicated #cardiovascular events were similar in both groups.
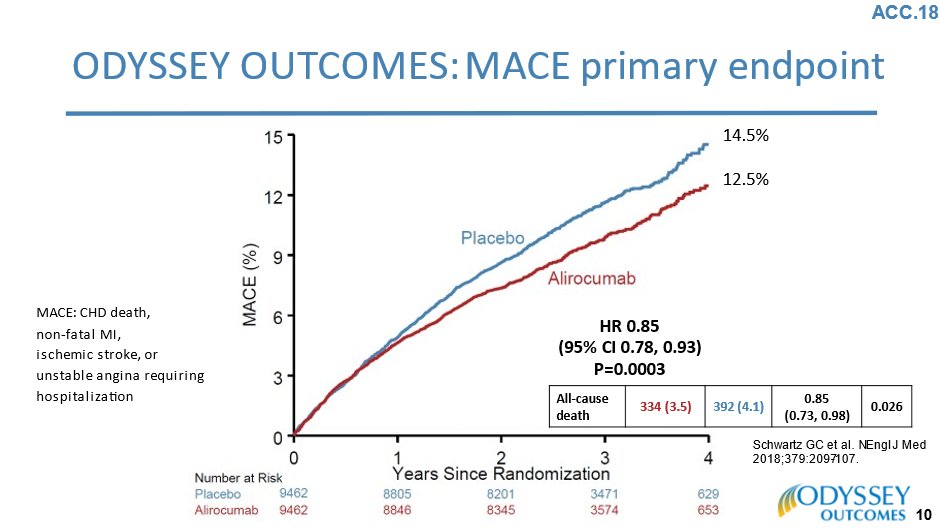
19) And then there's #alirocumab, studied in the #ODYSSEY OUTCOMES trial ( 🔓https://www.nejm.org/doi/10.1056/NEJMoa1801174): 18,924 patients who had previous #ACS & were receiving hi-intensity statin therapy. Median duration f/u 2.8y.
20) Composite primary end-point (#CHD death, nonfatal MI, ischemic stroke, or #UA req'ing hosp) was 12.5% in the alirocumab group vs 14.5% for placebo (P<0.001). AEs similar but for injection-site reactions w/ alirocumab.
21) Check out the great video summary at
22) So – in a post-MI patient, what should the LDL-C goal in such pts be?
23) Mark your best answer and then return TOMORROW for the correct response and a look at the other high-risk group at the center of this CE/#CME-accredited #tweetorial: #diabetics.
👏to @HeartBobH @JJheart_doc @AnnMarieNavar @JReinerMD @TedDodgeMD @MarcBonaca @MassGenBrigham
24a) Welcome back! YOU are earning 🆓CE/#CME while @cpcannon discusses aggressive treatment of elevated #LDL-C in the post-#MI and/or #diabetic patient. Yesterday we focused on post-MI; be sure to scroll back ⤴️if u missed anything, including the little quizlet in tweet 22!
24b) The answer? Well, it's a bit of a trick question: <55 is the “right” answer based on trials and @escardio #guidelines. It's <70 for the @ACCinTouch / @AHAScience guidelines. Biologically, lowest is best!
25) So now we turn our focus to amelioration of #ASCVD risk through #lipid-lowering therapies #LLT in patients with #diabetes. Many programs on @cardiomet_CE & @ckd_ce have highlighted the sheer magnitude of the #T2D "epidemic."
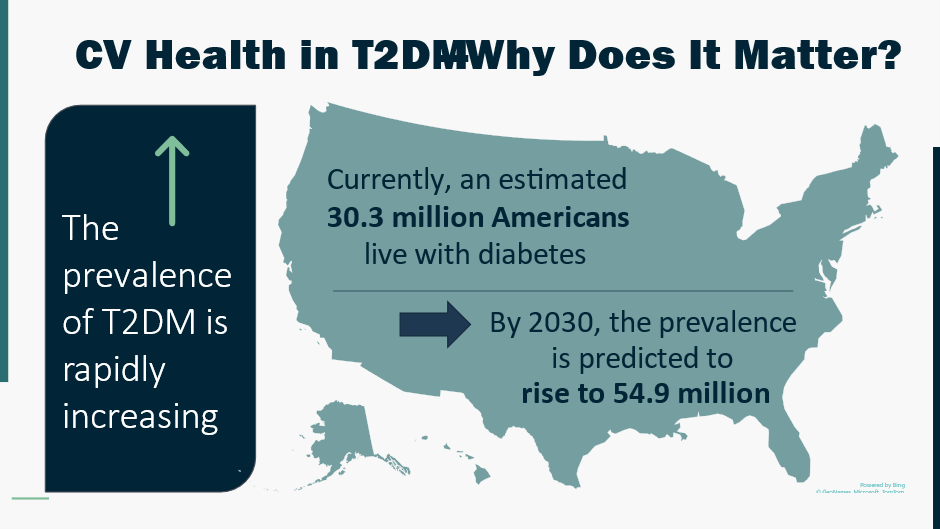
26) #Cardiovascular disease is, of course, the #1⃣ killer among patients with #diabetes. That makes it our prime target for potential risk reduction.
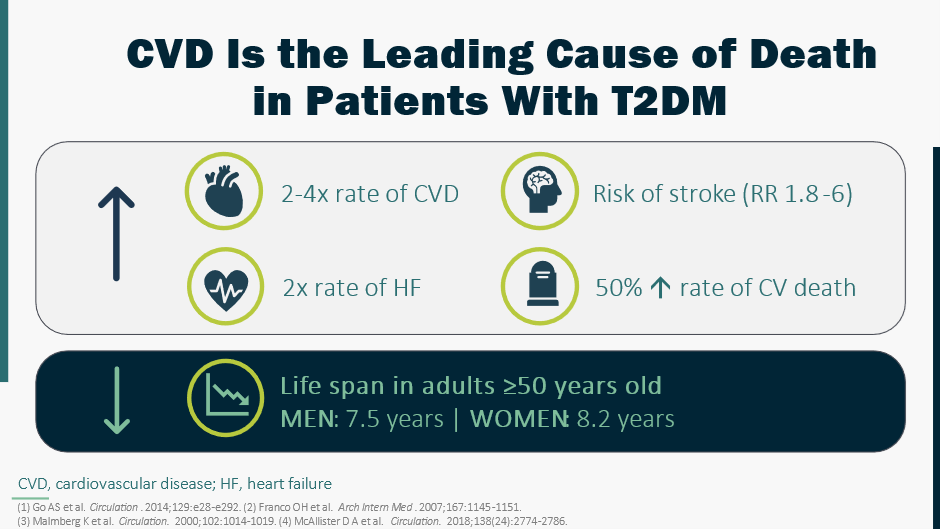
27) Patients with #DM are at high risk, & with #ASCVD become a “very high risk” patients, as seen in #FOURIER. Here's another secondary analysis: https://pubmed.ncbi.nlm.nih.gov/28927706/. At entry, 40% of pts had diabetes, 60% did not (though ~5/8 of those had #prediabetes.
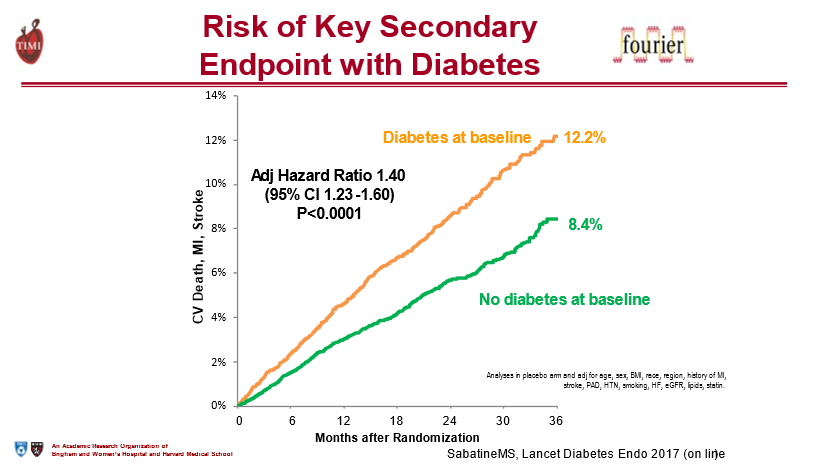
28) In FOURIER, evolocumab significantly ⬇️#CV outcomes consistently in both those with and without #diabetes, and the benefit seemed to be even greater with time in those with DM.
29) #Evolocumab did not ⬆️risk of new-onset diabetes, nor did it worsen glycaemia. The authors concluded that evolocumab use in patients with #atherosclerotic disease is efficacious and safe in patients with and without diabetes.
30) @AmDiabetesAssn management guidelines for #hyperlipidemia in diabetics are clear, and are aggressive:
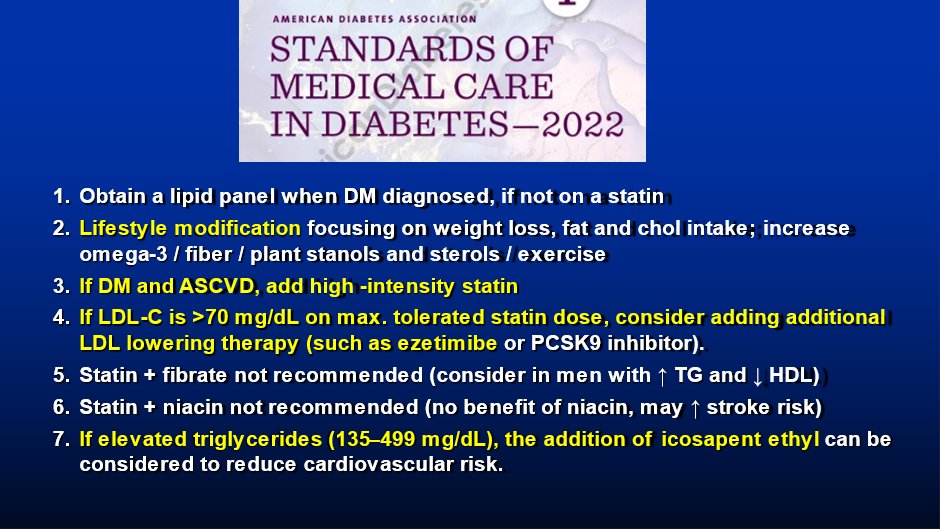
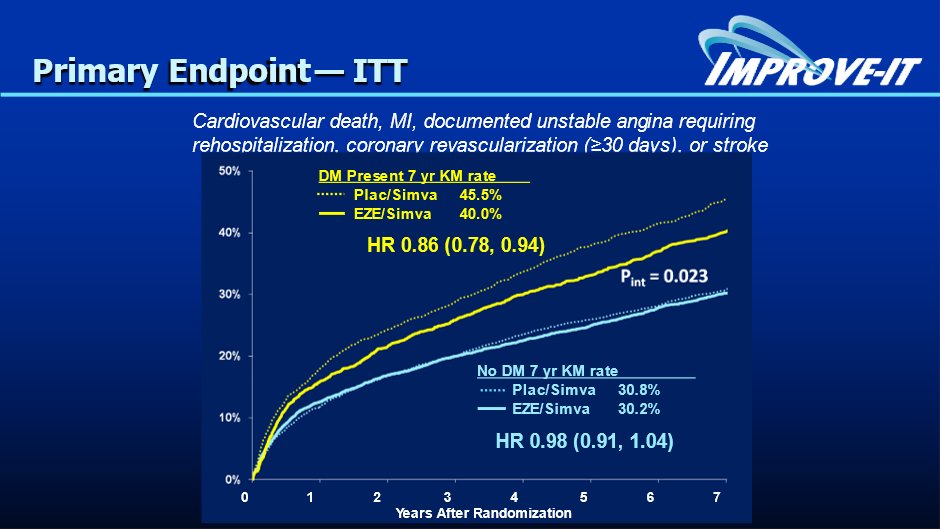
31) Data on patients with #diabetes in other #LLT trials also support the safety and the #ASCVD benefits of aggressive management. For example, in #IMPROVE-IT, @cardiomet_CE author @rgiugliano et al showed (🔓https://pubmed.ncbi.nlm.nih.gov/29263150/) that the benefit of adding #ezetimibe . . .
32) … to statin was enhanced in patients with #DM and in high-risk patients without DM. Interestingly, the 27% of trial pts w/ DM were more often older & ♀️, had had prior #MI & revasc, and presented more frequently with #NSTE-ACS compared with patients without DM.
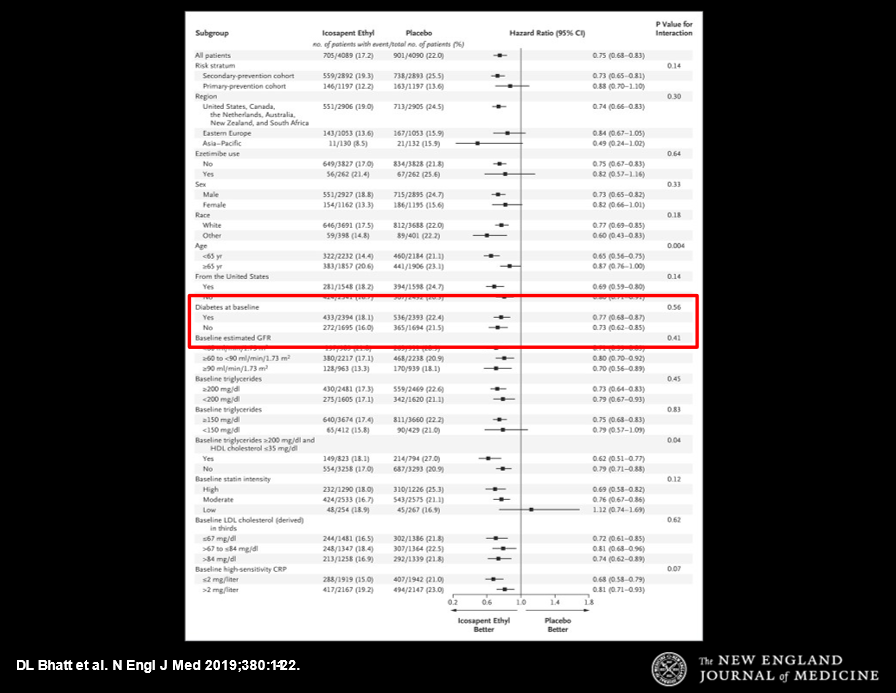
33) REDUCE-IT (🔓https://www.nejm.org/doi/full/10.1056/nejmoa1812792) was a large multicenter #DB placebo-controlled #RCT of pts with estab'd #CV disease or w/#diabetes & other risk factors, on statins, but with fasting #triglyceride of 135-499 and #LDL-C of 41-100.
34a) Pts received 2 g of #icosapent_ethyl BID or placebo. The primary end point was a composite of #CV death, nonfatal #MI, nonfatal #stroke, coronary revasc, or unstable angina. Results: pts on icosapent ethyl had sig ⬇️risk of ischemic events, including CV death . . .
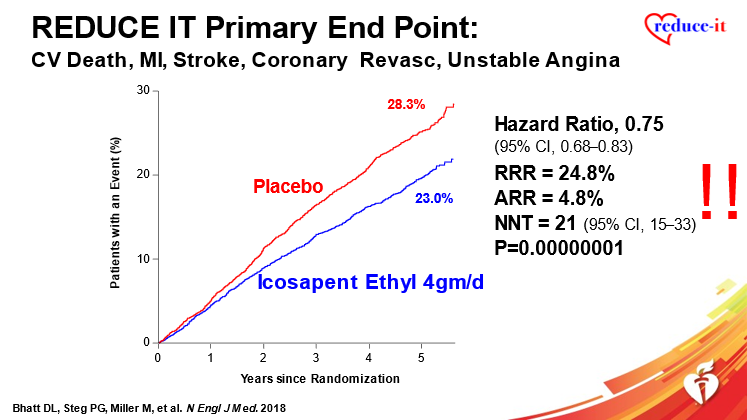
34b) . . . . and that was independent of whether or not patients had #DM at baseline.
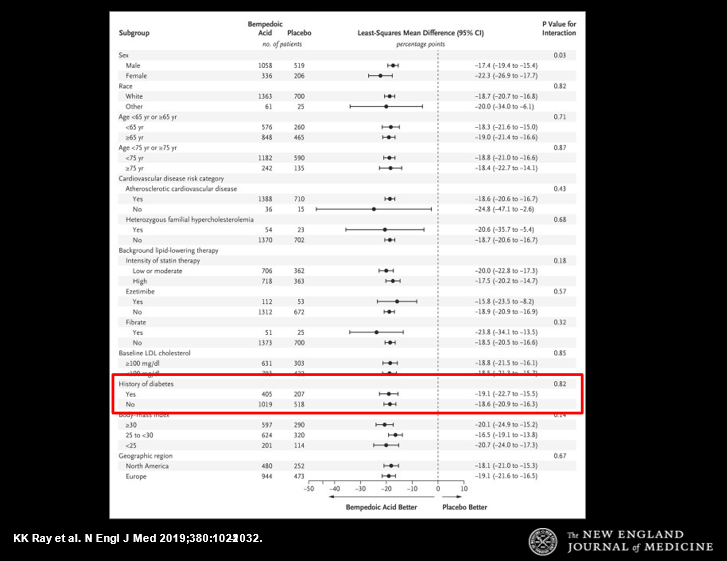
35) Likewise, in CLEAR HARMONY (🔓https://www.nejm.org/doi/full/10.1056/NEJMoa1803917) & in tweet 10 above), there was no difference between diabetics & non-diabetics re the efficacy of bempedoic acid + high-intensity statins in reducing LDL-C:
36) Thus, we are in an era of combination lipid lowering therapy. The evolution has been rapid – and is ongoing.
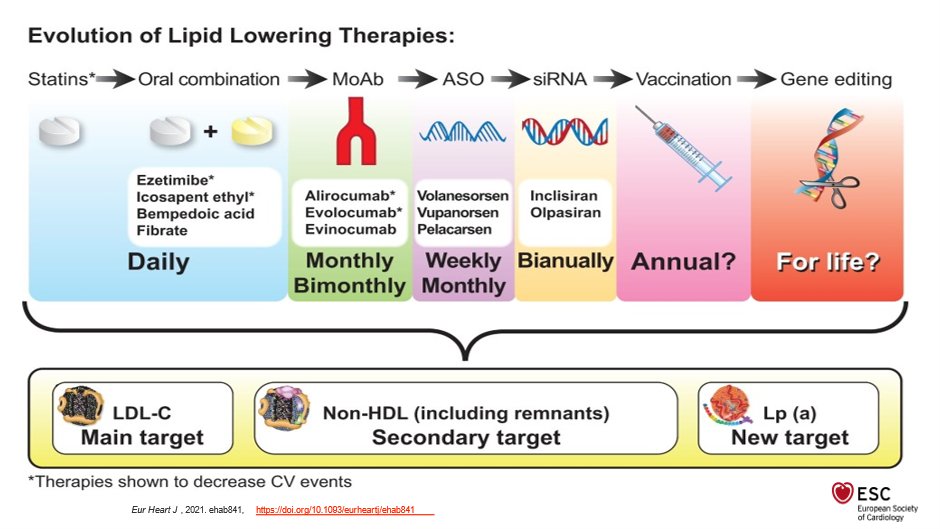
37) So what's ahead for these very high-risk patients? More and more sophistication: with DNA gene editing! (this is just entering human Phase I studies)
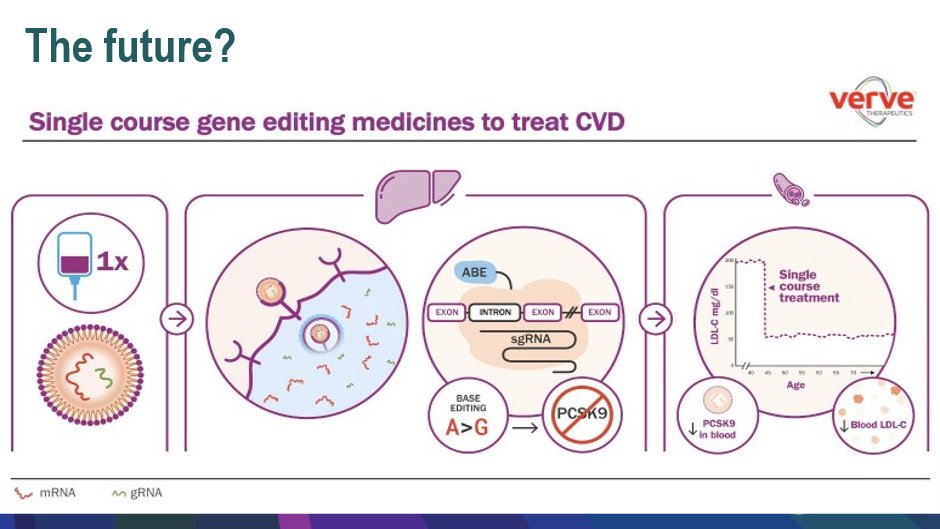
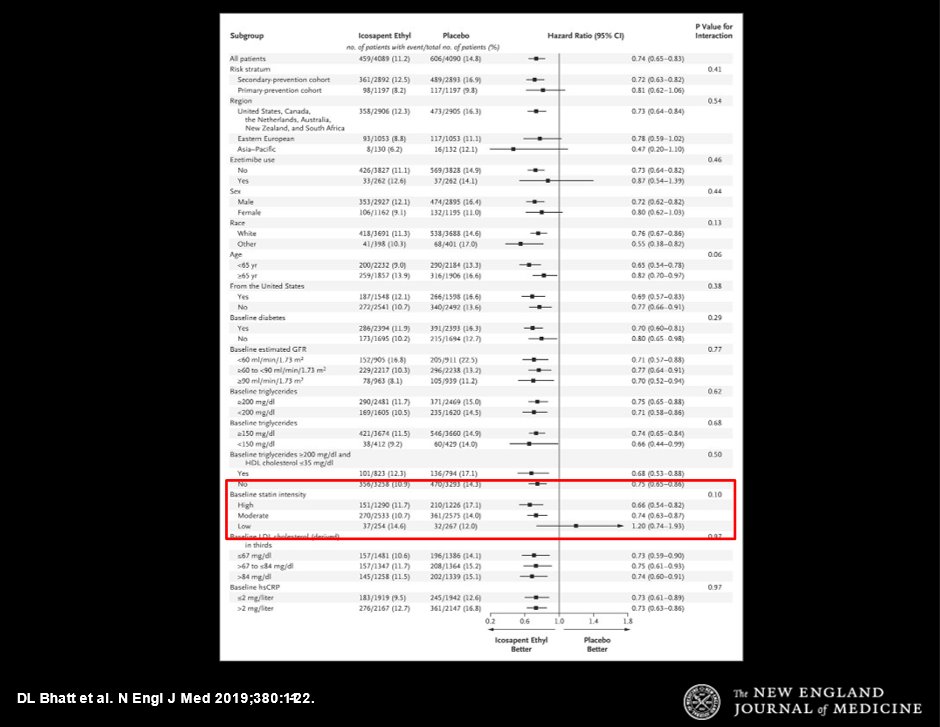
38) Except in frankly intolerant patients, however, #statins are still at the foundation of aggressive #LLT. In REDUCE-IT (tweet 33), what was the 1⃣subgroup that did NOT (by point estimate, not p-value) clearly benefit from addition of icosapent ethyl?
39) It’s the intensity of statin therapy (see box)!
40) Parting words:
41) And you have MADE IT! Titrate intensity of #LLT to severity of #ACSVD risk, and race to the bottom! It seems there is no such thing as TOO LOW when it comes to #LDL-C. Just like there's no such thing as TOO MUCH when it comes to 🆓CE/#CME!
42) So let's take a practice poll–not looking for a correct answer here: Do you treat an #ASCVD patient with #DM on high dose statin and #LDL 70, but #Trig 160 with additional combination rx?
43) So go now to https://cardiometabolic-ce.com/lipids5/ and grab your certificate—yes, it is that EASY. Shout outs to @AndrewJSauer @DrDebCroyNP @VietHeartPA @Lross246 @SnayCardsPharmD @biljana_parapid @drmalissawood @MichaelJBlaha @SamRRazaMD @DFCapodanno @anna_bortnick @smolock1 @drercardio
Originally tweeted by cardio-met (@cardiomet_CE) on April 26, 2022.
