1) Welcome to a new #accredited #tweetorial, Prevention and Management of Heart Failure in T2 Diabetes: The Diabetologist’s Perspective! Our expert author is Melanie J Davies CBE FMedSci @profmjdavies, Prof of Diabetes Medicine, U Leicester, Leicester Diabetes Unit @LDC_tweets

2) This program is intended for #healthcare professionals and is accredited by @academiccme for 0.75h CE/#CME credit for #physicians #physicianassistants #nurses #nursepractitioners #pharmacists 🇺🇸🇨🇦🇬🇧🇪🇺. FOLLOW US for #cardiometabolic education from expert authors!
3) @cardiomet_CE is supported by educational grants from AstraZeneca, Bayer, Boehringer Ingelheim Pharmaceuticals Inc. and Eli Lilly Company, and Chiesi. See archived programs still available for credit at http://cardiometabolic-ce.com. Disclosures at
3) In this programme we will consider evidence-based approaches to #manageHF & #preventHF in people living with #T2DM.
4) But let's begin with some basics, many of us are not #Hfexperts, but may be diabetes or primary care teams, so it's worth reminding ourselves of the typical #HFsigns and #HFsymptoms
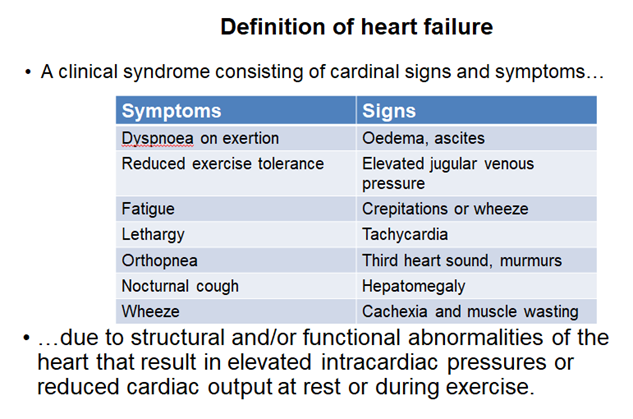
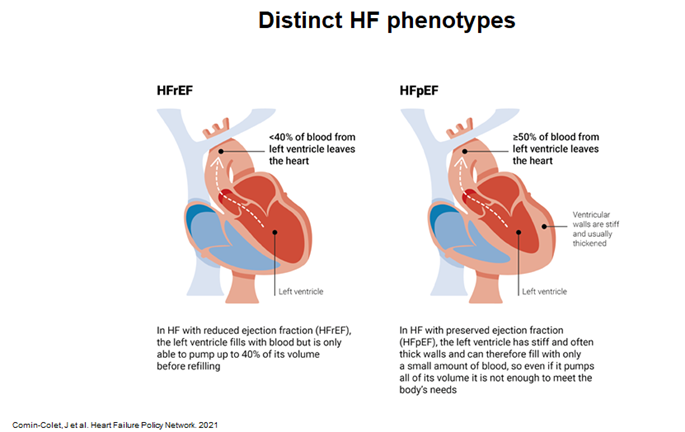
5) Also we increasingly recognise distinct #HFphenotypes based on #LVEF, for example Reduced Ejection Heart Failure #HFrEF & Preserved Ejection Heart Failure #HFpEF
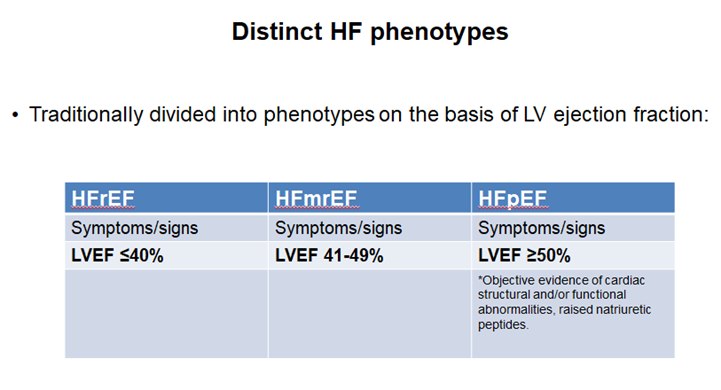
6) People with #diabetes comprise only about 5% of the entire adult population in the Western world, yet they account for 25-30% of admissions for #cardiovascular complications.
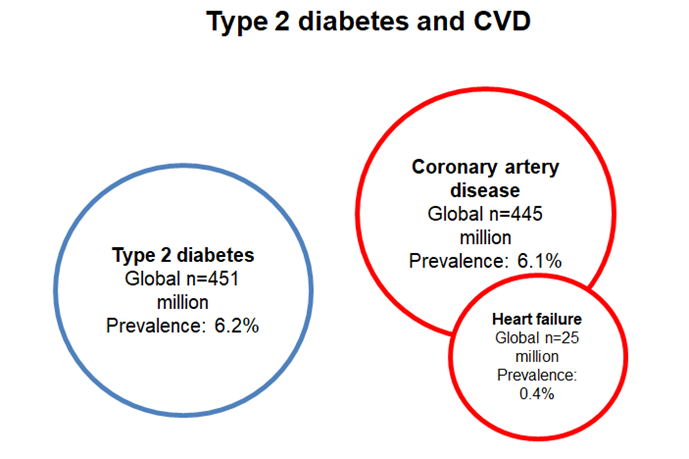
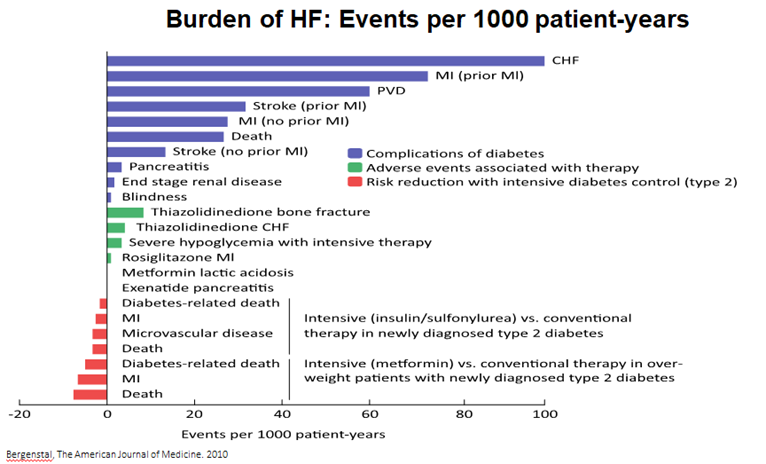
7) The high burden of #HF in #T2DM is starting to be more appreciated by #HCPs. For example, in https://pubmed.ncbi.nlm.nih.gov/20362759/, #HF had the highest number of events per 1000 patient years of any complication.
8) Although the signs and symptoms are the same, the mechanisms driving these are very different in #HFrEF and #HFpEF. See 🔓https://www.hfpolicynetwork.org/project/heart-failure-policy-summit-2021/ from @HFPolicyNetwork.
9) Furthermore, clinical outcomes for #HFrEF and #HFpEF are generally similar and are generally poor! See 🔓https://www.jacc.org/doi/abs/10.1016/j.jacc.2017.08.074.
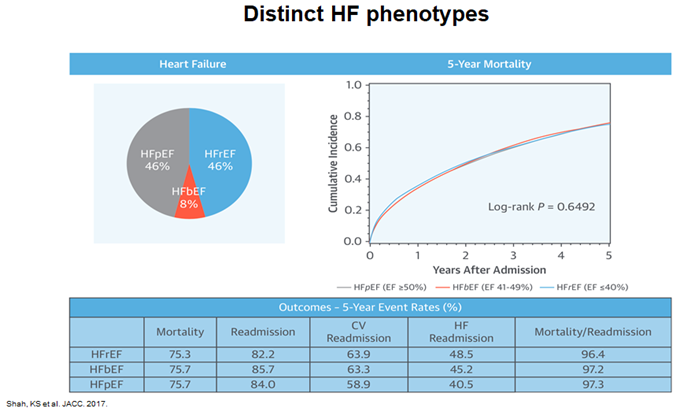
10a) In data from the “Get with The Guidelines – Heart Failure” (GWTG-HF) registry 🇺🇸 of patients presenting to hospital with acute decompensated heart failure, median survival overall was 2.1 years.
10b) In a risk-adjusted survival analysis, all subgroups had similar 5-year mortality and rehospitalization was similar for all subgroups.
11a) Mechanisms driving underlying #cardiac dysfunction are different in #HFrEF and #HFpEF. In the general population, patients with #HFpEF are more likely to be ♀️, with a higher prevalence of #hypertension and #diabetes. #Obesity is a major feature of HFpEF.
11b) By contrast, #HFrEF more commonly affects ♂️who have a history of ischaemic heart disease.
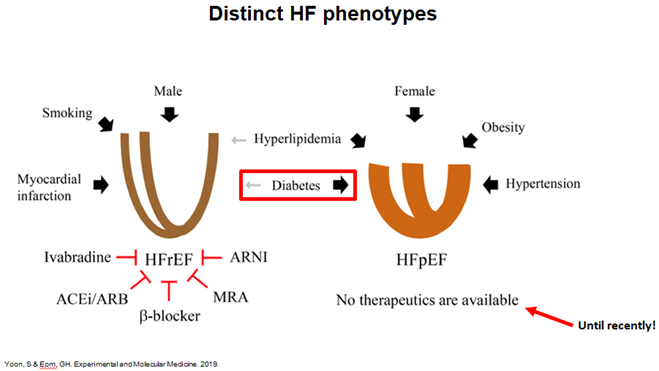
12) Moreover, remodelling patterns are different in the 2 forms of HF. The 🫀 in HFrEF is dilated, but in HFpEF is thickened & restricted. Most importantly, whilst there are many evidence-based tx's for HFrEF, until recently there have been no clear tx options for HFpEF.
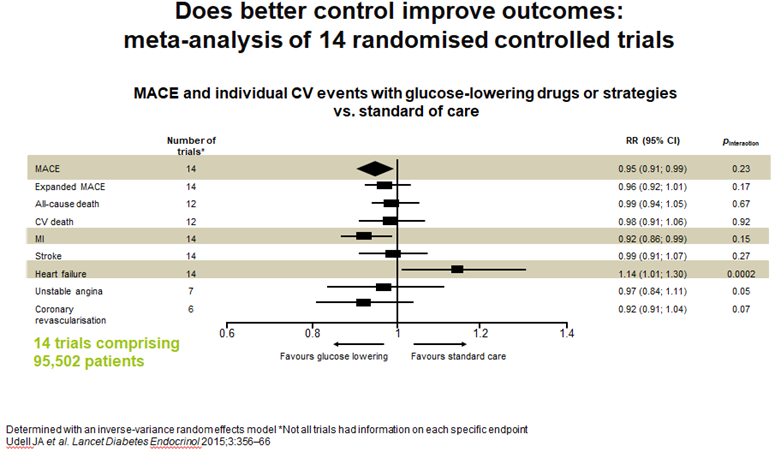
13a) See 🔓https://pubmed.ncbi.nlm.nih.gov/25791290/ for a meta-analysis of glucose lowering trials & impact on long-term outcomes that assessed the extent to which glucose ⬇️by various drugs/strategies affects risk of HF in pts w/ or at risk for T2D, …
13b) … & to establish whether #HF risk is associated with glycaemic control
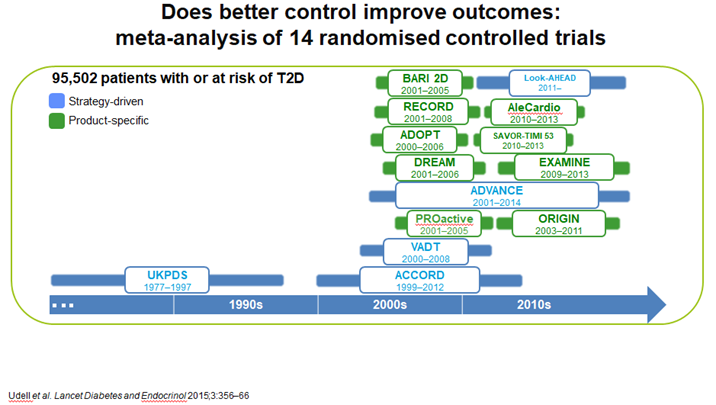
14) These data showed an ⬆️in #HF, probably explained by the inclusion of studies with #TZDs and the early trials with #DPP4i, including #saxagliptin
15) Furthermore, studies in those w/o #diabetes & risk of #HF, #HbA1c levels >5.5% are associated with incident heart failure, suggesting chronic hyperglycaemia prior to the development of #DM contributes to the development of #HF, highlighting the potential role of #prevention
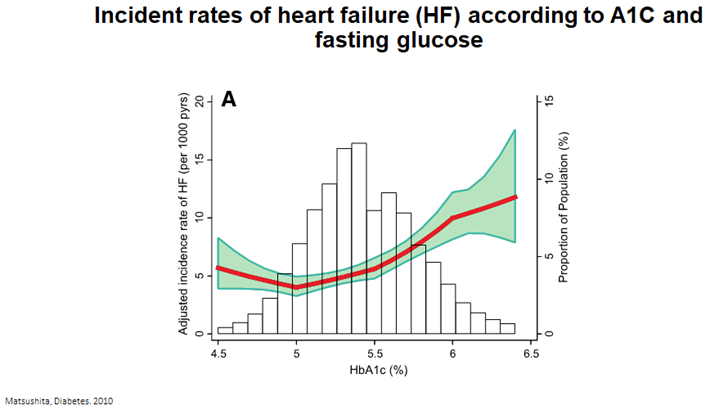
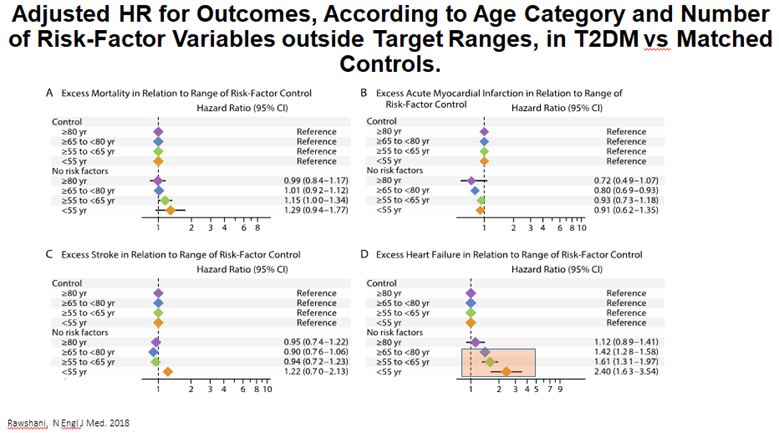
16a) The challenge of how to reduce the risk of #HF in people with #T2DM is highlighted in data from over 270,000 people with T2DM from the #Swedish National Diabetes Register 🇸🇪. Targeting 5 traditional #CV risk factors . . .
16b) . . . almost⬇️excess risk to control levels for #stroke & #MI but not #HF, partic in younger age groups. This emphasizes need for different approaches to care beyond traditional risk factor control to⬇️HF in #T2DM, esp in younger pts
17a) So what have we learned? Which of the following is MORE common in #HFrEF than in #HFpEF?
— cardio-met (@cardiomet_CE) May 10, 2022
17b) Mark your best answer & return TOMORROW for more education on the #prevention & #management of #HF in #T2D. EARN 🆓CE/#CME! 👍to @PNewlandJones @VickiaDSN @ClareHambling @WilmotEmma @EDEN_Leicester @drpratikc @sotonDSN @DrAndrewBaldwin @TaheriShahrad #FOAMed @kamleshkhunti
18) Welcome back! I am @profmjdavies and you are earning CE/#CME while you learn about #prevention & #management of #heartfailure in #T2D! Let's keep it going! 👏to @westernuFamMed @ProfBatterhamMD @AliRacaniere @JuleenRZierath @iDEALdiabetes @GoggleDocs @MedTweetorials #FOAMed
19) Yesterday's quiz? Scroll ⤴️to #17a if you didn't yet answer. NO PEEKING!
OK, the answer is d. patients with #HFpEF are more likely to be ♀️, with a higher prevalence of #hypertension and #diabetes. #Obesity is a major feature of HFpEF.
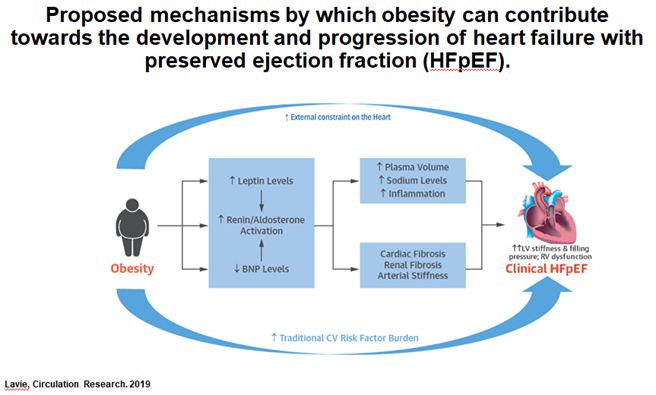
20) The mechanisms driving #HF in #T2DM are complex, multifactorial and incompletely understood, but ➡️ a particular predisposition towards #HFpEF.
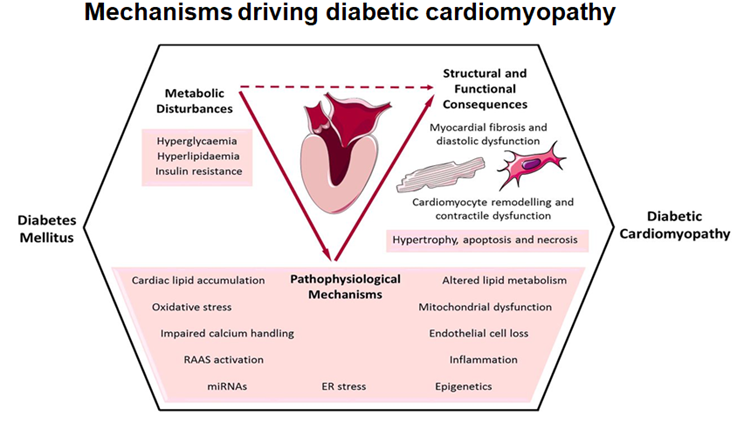
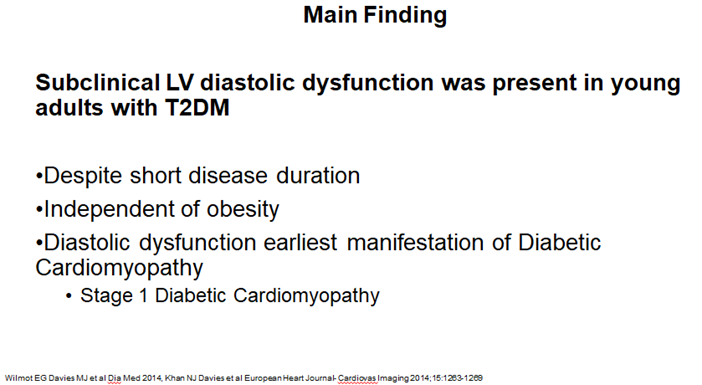
21) Data from our own group (see 🔓https://pubmed.ncbi.nlm.nih.gov/24606573/ & 🔓https://pubmed.ncbi.nlm.nih.gov/24970723/) highlights a real concern of the risk in early signs of heart failure in younger people with T2DM, beyond the risk with obesity alone

22) We showed Subclinical LV diastolic dysfunction was present in young adults with T2DM despite short disease duration & #Independent of #obesity. Indeed, #diastolic #dysfunction is the earliest manifestation of Diabetic #Cardiomyopathy (🔓https://pubmed.ncbi.nlm.nih.gov/24970723/)
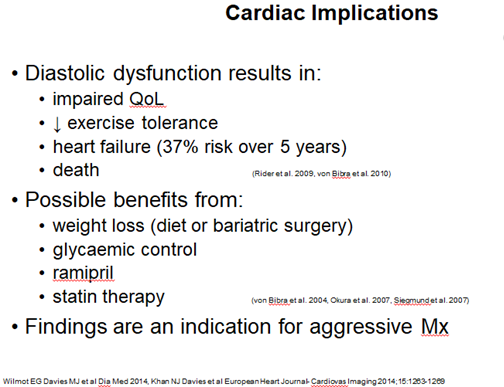
23a) Diastolic dysfunction results in impaired #QoL, reduced #exercise tolerance, #heartfailure (37% risk over 5 years). May get benefit from weight loss (diet or bariatric surgery), better glycaemic control, CV risk factor management including ACE inhibitors and statin therapy.
23b) That's the message from 🔓https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1768602/, 🔓https://pubmed.ncbi.nlm.nih.gov/17925474/, & 🔓https://pubmed.ncbi.nlm.nih.gov/18158708/). Diastolic dysfunction is an indication for early and aggressive management including potential for weight management in this younger and high risk group
24a) Moving to what we know regarding #HF outcomes for the trials of various #GLT (glucose lowering therapies) in #T2DM, we can categorise agents that increase risk of #HF – the #TZD & some of the #DPP4i’s (saxliptin).
24b) Other #DPP4i, #basal #insulin, and α-GI are neutral but and @glp1 RAs have modest benefit from meta-analysis. #SGLT2i show consistent and robust benefits. Consider 🔓https://www.nejm.org/doi/full/10.1056/nejmoa1504720, 🔓https://pubmed.ncbi.nlm.nih.gov/30418475/, 🔓https://pubmed.ncbi.nlm.nih.gov/28605608/, 🔓https://pubmed.ncbi.nlm.nih.gov/30415602/. . .
24c) 🔓https://pubmed.ncbi.nlm.nih.gov/28910237/, 🔓https://pubmed.ncbi.nlm.nih.gov/26630143/, 🔓https://pubmed.ncbi.nlm.nih.gov/27633186/, https://pubmed.ncbi.nlm.nih.gov/30291013/, 🔓https://www.nejm.org/doi/full/10.1056/nejmoa1203858, https://pubmed.ncbi.nlm.nih.gov/28917545/, 🔓https://pubmed.ncbi.nlm.nih.gov/26052984/, https://pubmed.ncbi.nlm.nih.gov/25765696/, 🔓https://pubmed.ncbi.nlm.nih.gov/23992601/ . . .
24d) 🔓https://pubmed.ncbi.nlm.nih.gov/17666462/, & https://pubmed.ncbi.nlm.nih.gov/19501900/, 🔓https://pubmed.ncbi.nlm.nih.gov/27295427/. So, you're welcome–there's your #HF—#T2D clinical trial library!
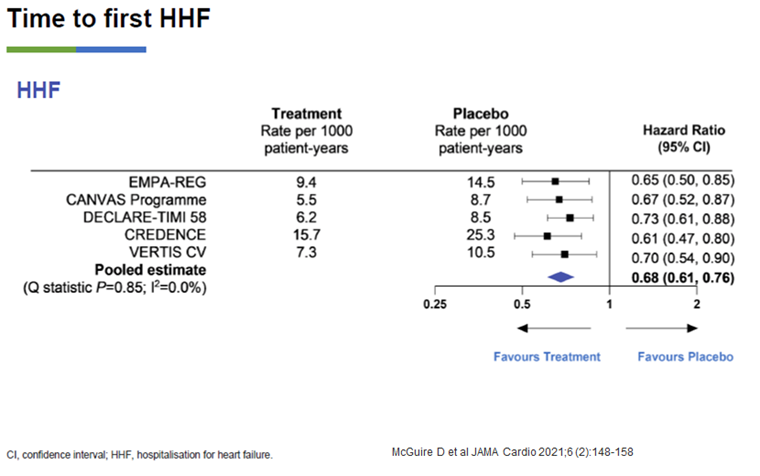
25) Data from the large #CVOTs in #T2DM with the #SGLT2i class has shown robust & remarkably consistent benefit in reducing hospitalisation for Heart Failure #HHF, a pre-specified secondary outcome in many of these trials
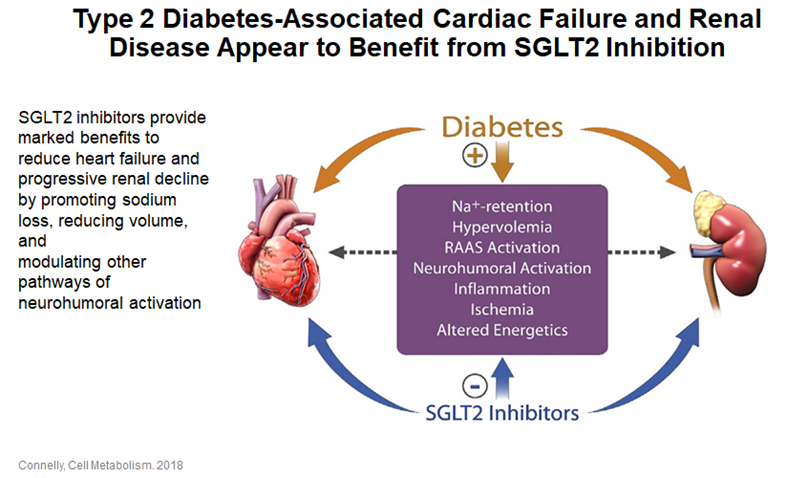
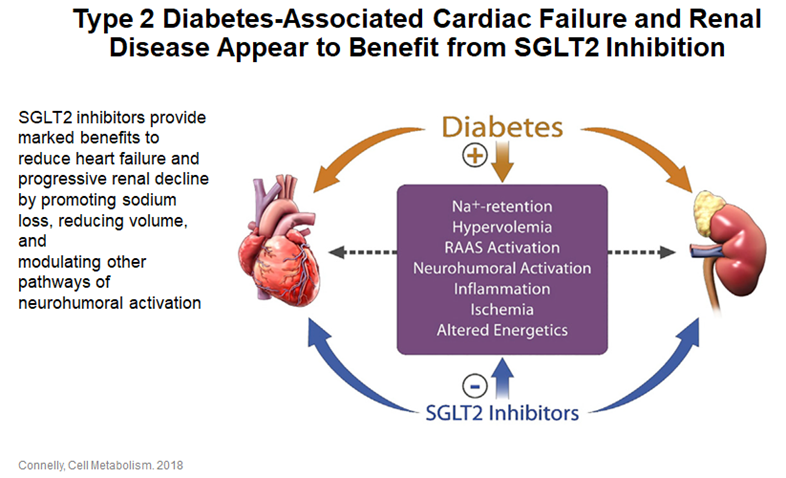
26) There are a number of postulated mechanisms which explain the beneficial effects of #SGLT2i on #heartfailure outcomes & also explain their benefit in #CKD
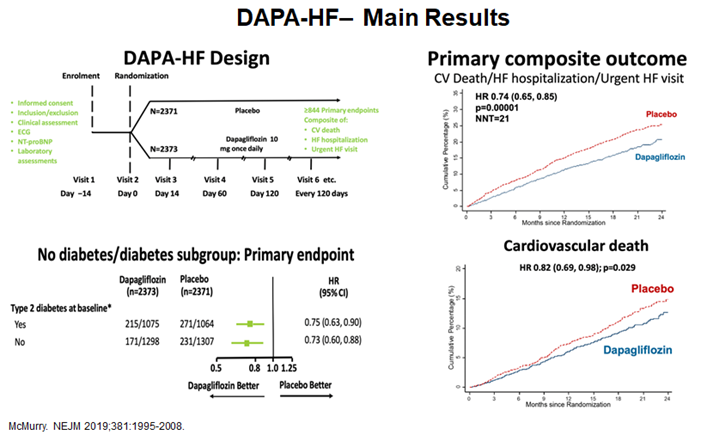
27a) The first trial to examine #HF as a primary outcome in people w/ & w/o #T2D was the #DAPA_HF study with #Dapagliflozin (🔓https://pubmed.ncbi.nlm.nih.gov/31535829/). The trial met its primary endpoint of CVDeath/hHF/UrgentHF visit as well as showing ⬇️#cardiovascular death with dapagliflozin.
27b) DAPA-HF was the 1st HF outcomes trial investigating tx of adults with #HFrEF, w/ & w/o #T2D, w/ an #SGLT2i on top of standard of care (#ACE-I, #ARB, β-blockers, #MRA, #ARNI). Dapa➡️stat significant & clinically meaningful⬇️in risk of worsening heart failure events …
27c) … and #CV death vs placebo, ➕improvement in #HFsymptoms, when added to standard tx. The safety findings of DAPA-HF were consistent with the well-established safety profile of dapagliflozin and the rate of discontinuation was low.
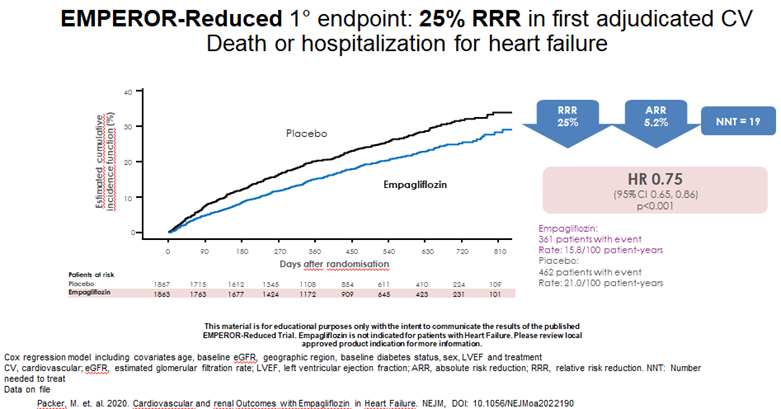
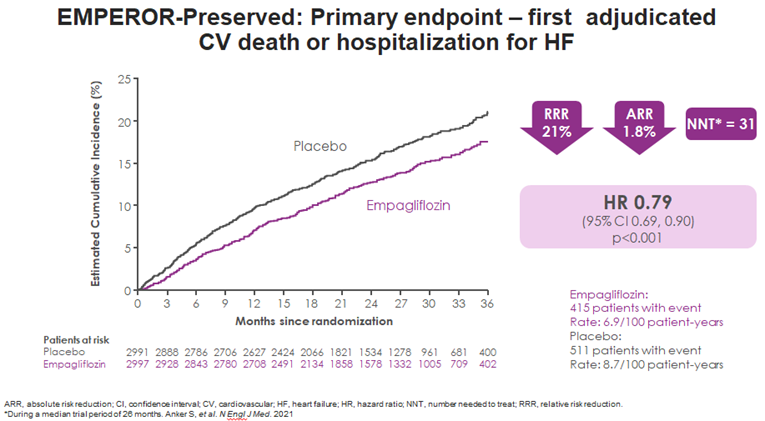
28) A subsequent #HF trial with the #SGLT2i #Empagliflozin also met its primary endpoint: 🔓
30) So how about a quick knowledge ✔️? Which of the following helps explain the benefit of #SGLT2i therapy on #HF & #CKD outcomes?
— cardio-met (@cardiomet_CE) May 11, 2022
31) Mark your best answer and return tomorrow for a wrap-up of this program and a link to your 🆓CE/#CME! It's that easy! Tip o' the hat to @EsePresident @brendonneuen @RpratleyMD @AliceYYCheng @cpcannon @DLBHATTMD @SantosGallegoMD @mvaduganathan @EylemLevelt @ShivaniM_KC
32) Hooray! You're back! I am @profmjdavies & you have a few educational morsels left to enjoy before you grab your CE/#CME certificate! Shout-outs to @DanielJDrucker @busediabetes #cardiotwitter #nephtwitter #endotwitter
As to yesterday's quiz–it's C! Remember this from #26?
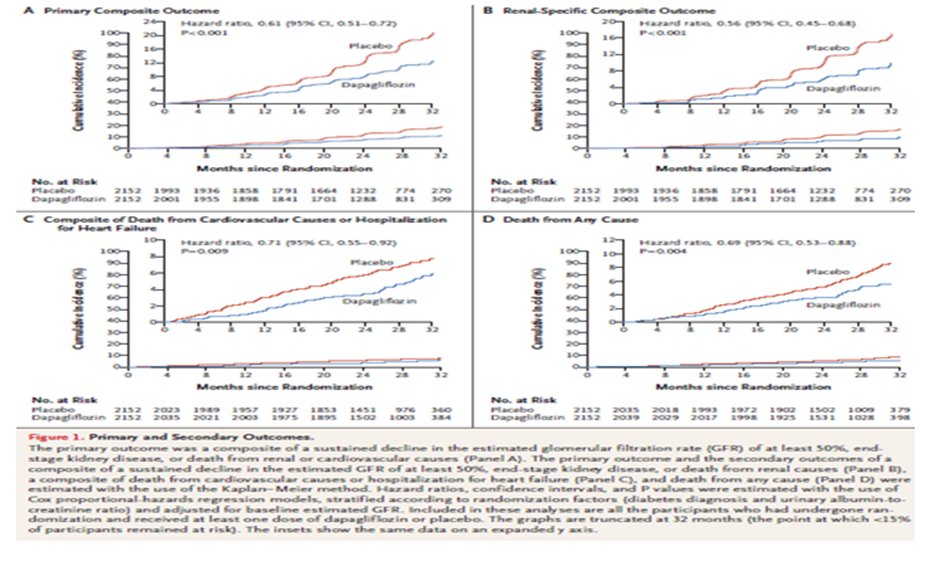
33) As #heartfailure and chronic kidney disease #CKD are often inextricably linked, it is not surprising that in the first outcome trial for CKD in people regardless of the presence or absence of diabetes #DAPACKD …
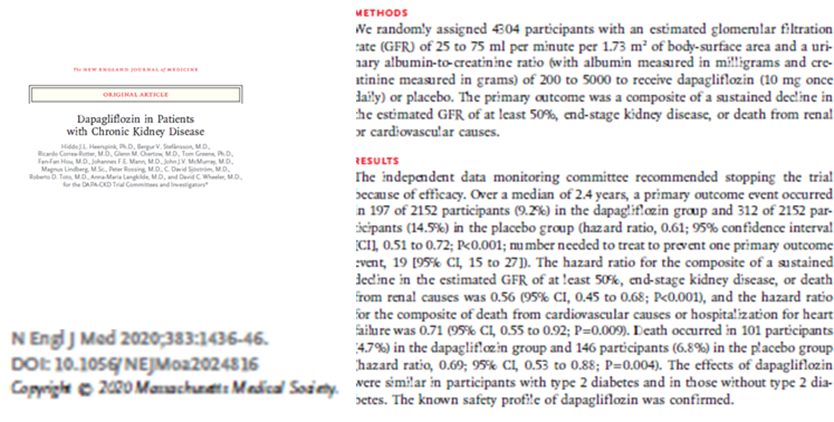
34) … the trial showed benefits in #CKD outcomes but the composite outcome of death from #cardiovascular causes or hospitalization for HF #HHF were also reduced HR 0.71 (95% CI 0.55-0.92)
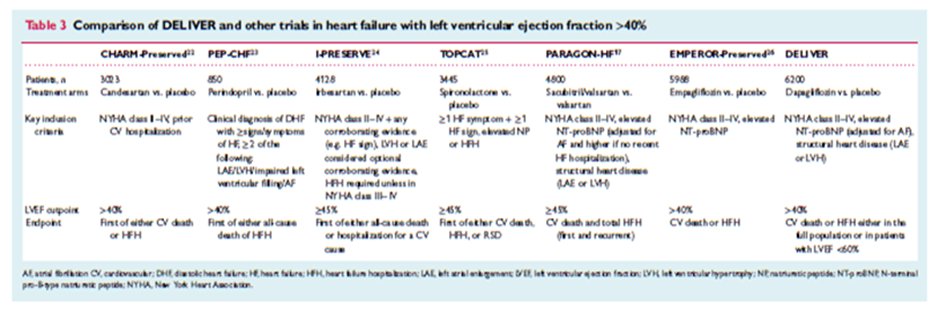
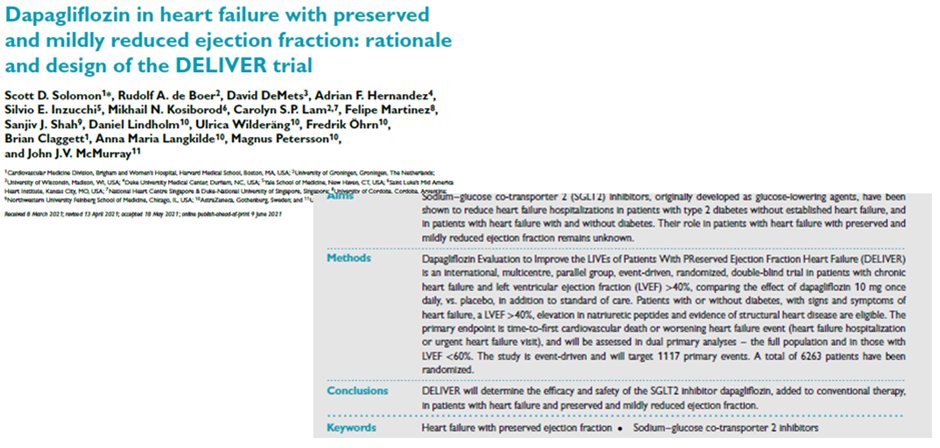
35) A particular challenge has been finding effective treatments for #HFpEF. Trials in this area include CHARM-Preserved, PEP-CHF & I-PRESERVE with #ACE and #ARBs, & there are 2 outcome trials with #SGLT2i: #EMPEROR-Preserved (empagliflozin) & #DELIVER (dapagliflozin)
36) EMPEROR-Preserved has recently reported (🔓https://pubmed.ncbi.nlm.nih.gov/34449189/) and met its primary endpoint, a composite of #CVdeath or #hHF
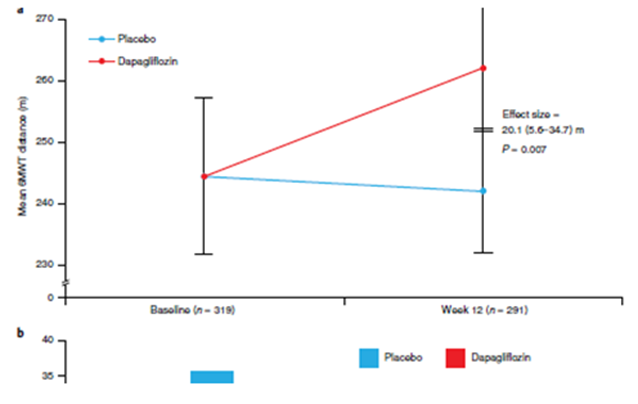
37) Interestingly, a smaller & shorter-duration trial with dapagliflozin explored the impact of #DAPA on functional outcomes & #QoL in people with #HFpEF. This is important as HFpEF has a high burden of symptoms and poor QoL.
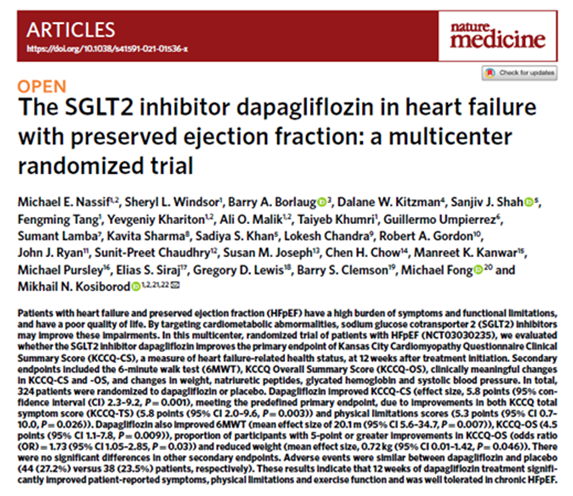
38) In this study 🔓https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8604725/, dapagliflozin was shown to improve functional outcomes and QoL as assessed by the #KCCQ (Kansas City Cardiomyopathy Questionnaire
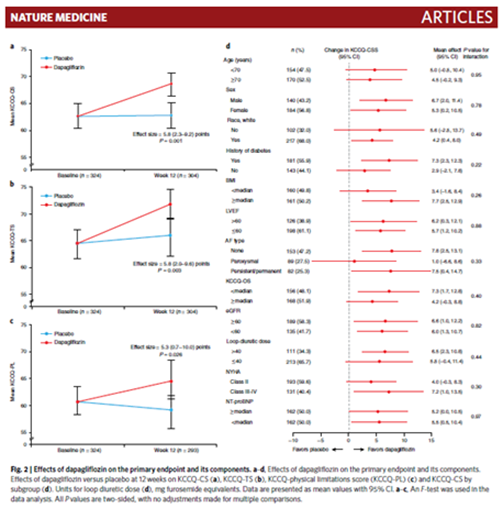
39) Of particular note was the impact that dapa had on the 6-minute walk test #6MWT, a good marker of functional status. This improved at 12 weeks by 20.1m (p=0.007), proportionally a large⬆️ (8.2%) given the low baseline level (244.4m).
40) The larger outcome trial with #dapagliflozin in #HFpEF is ongoing
41) #Obesity is thought to play a key role on the pathogenesis of #HFpEF and there are also ongoing trials of #GLP1 RAs such as #semaglutide, which will provide further insights in the role of these agents in HFpEF
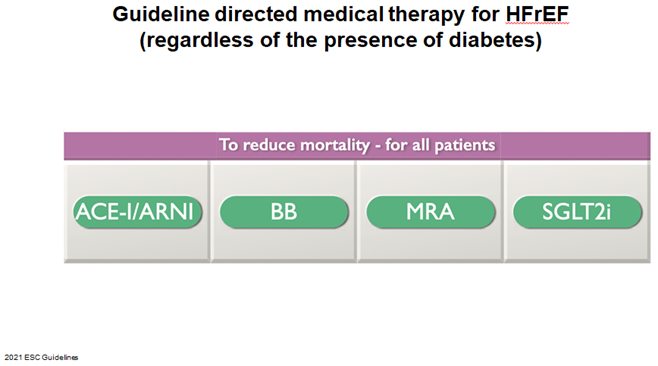
42) Moving to the management of #HF the 2021 ESC Heart Failure include the use of ACE-I/ARNI, Beta Blockers, and MRA, and now #SGLT2i in all people with #HFrEF regardless of the presence of #DM. 🔓
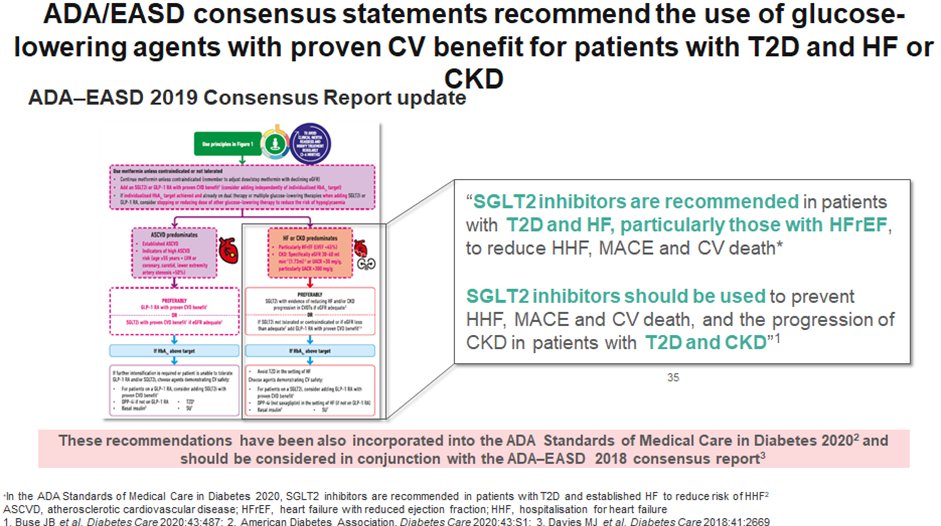
43) 2019 Update to Management of Hyperglycemia in Type 2 Diabetes, A Consensus Report by the American Diabetes Association (@AmDiabetesAssn ) and the European Association for the Study of Diabetes (@EASDelearning) also highlight that #SGLT2i are preferred agents in #HFrEF
44) Key takeaways from @profmjdavies include
👉Heart Failure is increasingly recognised as an important co-morbidity which is difficult to manage
👉CVOTs with glucose lowering agents show between & within class difference in #cardiorenal protection, ⬇️#CVdeath, & effect on HF
45)
👉New data emerging on the benefits of #SGLT2i in #HFpEF including on functional outcomes & #QoL
👉#SGLT2i are the preferred class of glucose-lowering therapy #GLT for reducing the risk of #heartfailure
46) And that's it! You've made it! Hopefully you learned much and you will click on https://cardiometabolic-ce.com/cardiorenal18/ so that you can claim your #CE/#CME certificate! I am @profmjdavies and I encourage you to follow @cardiomet_CE for the best, most accessible education from the experts!
Originally tweeted by cardio-met (@cardiomet_CE) on May 10, 2022.
